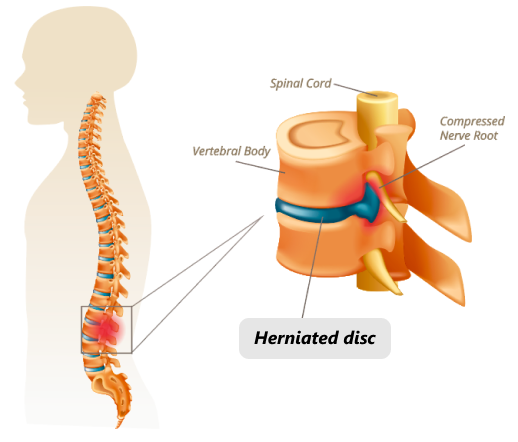
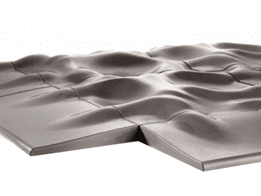
Intervertebral discs serve as spacers and shock absorbers between the vertebrae of your spine. They prevent bones from rubbing together and provide a space for nerve roots to exit the spinal canal and travel to structures throughout your body.
The discs are made up of a tough rubbery exterior called the annulus, and a soft center called the nucleus. The annulus is composed of fibrous layers of collagen and proteins, while the gel-like nucleus is made up of mostly water and collagen. The discs give your spine its mechanical flexibility and shock-absorbing properties.
A disc can become ruptured, or herniated, when a portion of the nucleus bulges through a crack in the annulus. Most herniated discs occur in the lower back, but they can also arise in the neck. A herniated disc can be asymptomatic if it does not affect a nerve. But when a bulging disc compresses a nerve root where it exits the spinal column, it can cause severe pain and restricted mobility.
Herniated discs are common among adults. In fact, Most people after age 40 have some degree of bulged and herniated discs, and foraminal compressions to the spinal nerve roots. The majority of them are asymptomatic, producing no pain at all, and where pain is present, herniated discs are often not the sole generators of pain.
Pain is often caused by a combination of soft tissue lesions, pelvic /hip misalignment, ligamentous and fascial deterioration, muscular trigger points, and cutaneous nerves entrapment within the toraco-lumbar fascia. Unfortunately, MRI does not show those details, and doctors often focus on disc lesions, unaware of other factors that contribute to disc herniation.