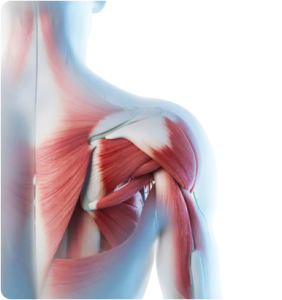
Your rotator cuff is a group of four muscles and their tendons that surround and cover the shoulder joint. The muscles hold the head of the humerus (upper arm bone) firmly in place within the shoulder’s shallow socket, and attach the humerus to the shoulder blade, providing stability and governing shoulder movement.
The rotator cuff makes it possible to freely lift, lower and rotate the arms in all 3 planes of motion, making the shoulder the most mobile joint in the human body. Unfortunately, the tradeoff for high shoulder mobility is wear-and-tear of the rotator tendons – especially the supraspinatus, as it has to glide beneath the subacromial space, which has a complex anatomy.
Rotator tendon ruptures are common in sports, especially those that require shoulder rotation and overhead movement, like swimming, tennis, baseball and other sports that place a high demand on the shoulder joint.
The shoulder is a ball-and-socket joint made up of three bones: the humerus (upper arm bone), the scapula (shoulder blade), and the clavicle (collarbone).
The head (ball) of the humerus fits into a shallow socket in the shoulder blade.
Your rotator cuff is formed by a group of four muscles and their tendons. They originate at your scapula and wrap around your glenohumeral joint, or shoulder. The supraspinatus runs from the scapula (shoulder blade) to the greater tubercle of the humerus, and works to abduct the arm and shoulder.
The subscapularis runs across the top and front of the humeral head, and works to rotate the shoulder forward and inward.
The external rotators – infraspinatus and the teres minor – run across the back of the humeral head and allow you to raise your arm overhead and rotate your shoulder outward.
The supraspinatus primarily abducts the shoulder, but can also internally rotate it when the humerus is in an internally rotated position
The rotator cuff muscles are anchored to the head of your humerus by tough tendons that stabilize the shoulder joint and hold the humerus in place within the glenoid fossa. The rotator cuff complex is protected by bursae in each shoulder that prevent the soft tissues from rubbing against bone.
Your rotator cuff enables you to execute finely tuned upper body movements. A stable and mobile shoulder joint is particularly important in sports like tennis, baseball, swimming and football, where precise shoulder movement is critical for elite skills execution.
The rotator cuff tendons often undergo degenerative changes after the age of 55 as a normal part of the aging process.

Factors that contribute to rotator tendon degeneration include:
Aging tendons also lose elastin, making them less elastic and increasing the risk of tears during physical activity. Loss of muscle strength in the shoulder complex and poor posture cause a decrease in the subacromial space, and excessive friction, compression and overload of the rotator cuff tendons promote tendon degenerative changes.
The aging supraspinatus tendon can thicken and become soft, preventing it from gliding in the subacromial space, and causing impingement that eventually leads to partial-thickness tears.
The shoulder’s diverse, multiplanar range of motion makes the rotator cuff highly vulnerable to a variety of injuries. This is particularly true in sports and occupational activities that demand repetitive use of the arm and shoulder.
Common rotator cuff injuries include:
Common causes of non-athletic rotator cuff injuries include wear and tear that weakens the tendon, lack of physical activity (disuse), smoking, extending the arm during a fall, and repeated steroid injections that deteriorate tendon tissue.
Rotator cuff tears are often categorized by origin and degree. While there are many subcategories of tearing, the four main types we see most in our clinic include:
Full-thickness tears: The worst kind of rupture, a complete tear splits the soft tissue into two separate pieces, or detaches the tendon from the bone. In the worst cases, the tendon cannot be fully repaired, and function is only partially restored. Partial thickness tears: Partial thickness rotator cuff tears (PTRCTs) are graded by the length of the tear, with tears less than 3mm being grade 1, tears 3mm to 6mm being grade 2, and tears greater than 6mm being grade 3. PTRCTs are further categorized by location: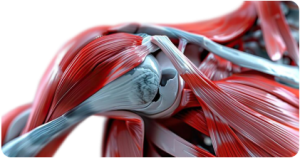
Other factors that play into categorization of PTRCTs are tissue quality, direction of tearing (anterior-posterior or medial-lateral), and the etiology (cause) of the tear.
All sports have inherent risks, but certain sports have a higher incidence of rotator cuff injuries:
Athletes should not ignore rotator cuff pain, as injuries may worsen over time. Early diagnosis and treatment are key to successful recovery and return to play.
or
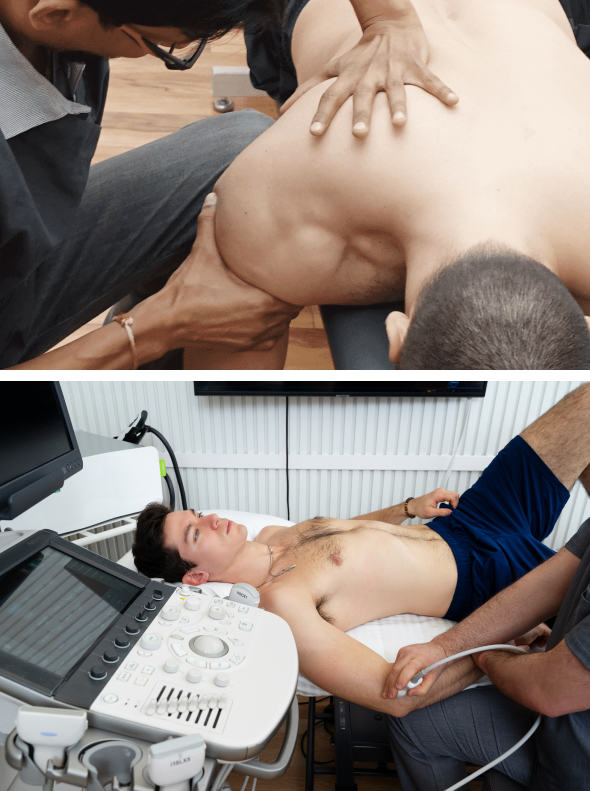
Dr. Kalika, clinical director of NYDNRehab, has devoted his life’s work to finding innovative and effective ways to treat musculoskeletal pain and dysfunction. Dr. Kalika has published multiple scientific articles on the use of musculoskeletal ultrasonography in rehabilitative medicine. He has developed his own holistic methodology for diagnosing shoulder and rotator cuff pain with the use of high-resolution ultrasound imaging.
According to Dr. Kalika, shoulder pain is too often mismanaged, focusing on the rotator cuff while ignoring the scapula. Physical therapy is most effective when the structural integrity of scapular muscles and nerves is restored. Regenerative therapies for rotator cuff tendons yield only mediocre results if the shoulder girdle/neck complex is not addressed holistically. Dr. Kalika’s diagnostic approach includes a dynamic exam of the shoulder and scapular muscles using motion analysis technology and ultrasound imaging.
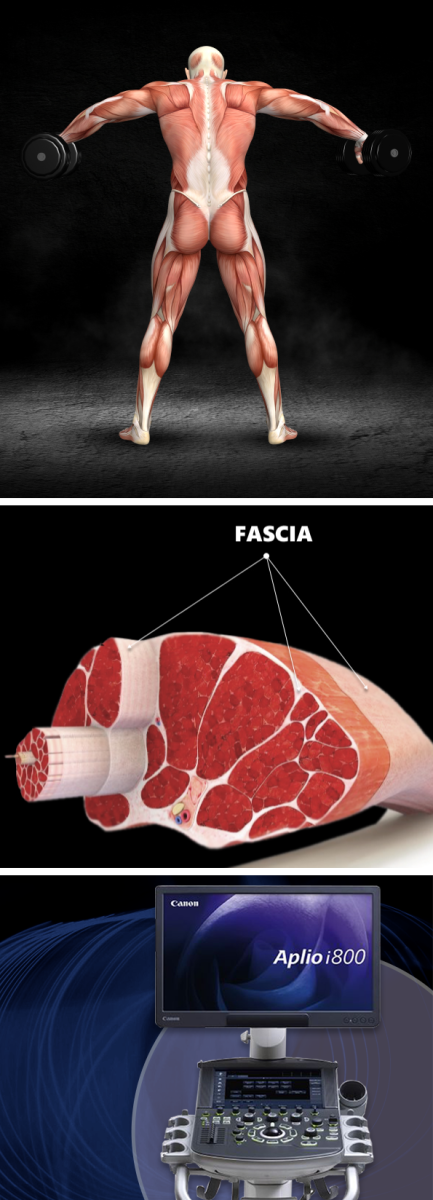
Dr. Kalika is at the forefront of pioneering work on fascia, the connective tissue that encases and connects muscles and organs throughout the body. Fascia plays an important role in stabilizing the shoulder joint, permitting nerves and blood vessels to glide freely among other structures. Dr. Kalka uses high-resolution ultrasound to visualize fascia connections that affect shoulder function. He is certified in the Stecco method of fascia manipulation, an approach that targets fascia densifications that impede shoulder movement.
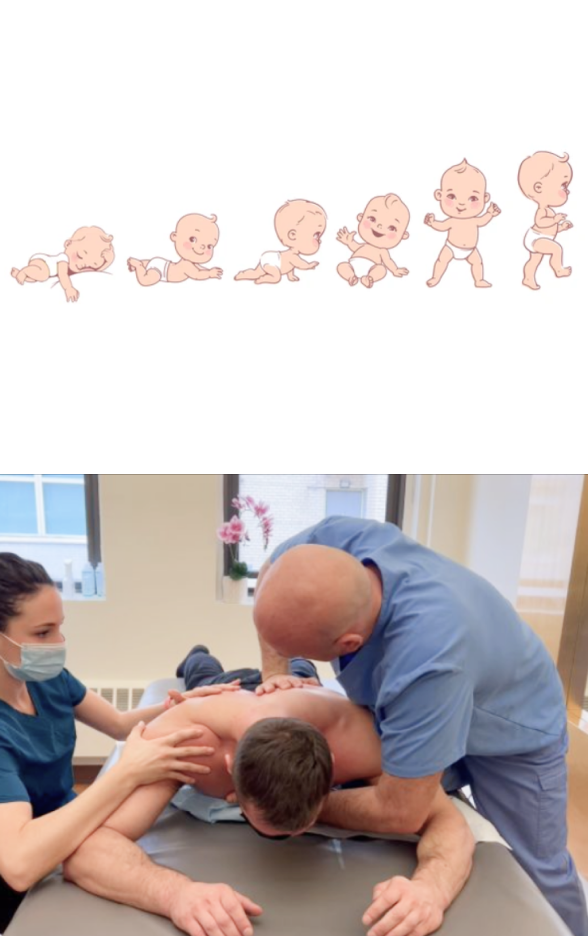
Dr. Kalika studied directly under Dr. Ben Kibler, world-renowned orthopedic surgeon and pioneer of scapular dyskinesis. His diagnostic approach focuses on the structural integrity of the scapular muscles, and the nerves that innervate the shoulder complex. He addresses these issues with regenerative therapies, orthobiologic procedures, and specialized physical therapy.
Dr. Kalika was among the first in his field to become certified in dynamic neuromuscular stabilization (DNS), the most integrative evidence-based approach to treating shoulder pain. He was mentored directly by the creator of DNS, Dr. Pavel Kolar. His expertise in treating athletic rotator cuff injuries is unsurpassed in NYC.
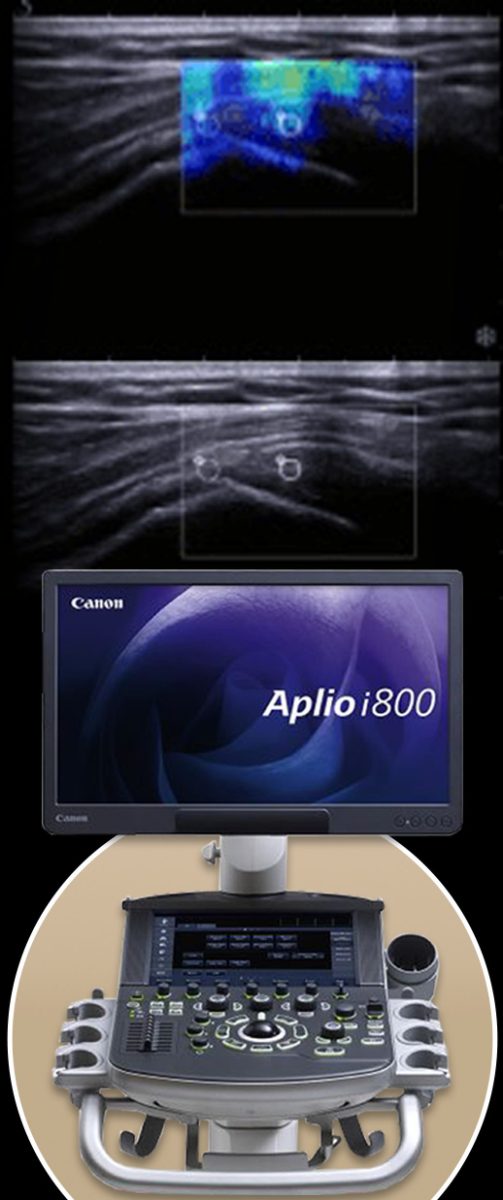
The complexity of the shoulder region makes it challenging to accurately identify the exact source of shoulder pain and dysfunction. A clinical exam with testing for strength and range of motion can help to narrow down possible causes, but ultrasound imaging is necessary to get an accurate diagnosis of rotator cuff dysfunction.
Diagnosis of shoulder pathology often relies on reported symptoms and findings from a clinical exam, but that approach may overlook critical aspects of your injury, resulting in mistreatment, prolonged pain, and excess medical costs. Dynamic ultrasound imaging lets us visualize the big picture in real time, with the shoulder in motion.
With diagnostic ultrasound, we can:
In addition to high-resolution imaging, our advanced equipment has capabilities for sonoelastography to gauge tendon stiffness, and superior microvascular imaging, to detect early signs of healing and monitor patient progress.
Ultrasound imaging takes the guesswork out of diagnosis, enabling us to quickly identify and treat multiple factors that contribute to rotator cuff dysfunction. Your on-site ultrasound exam takes place on your very first visit, in the comfort of our clinic. Quick and accurate diagnosis means you can begin therapy right away, with no wait time for lab results.
For years, MRI has been considered the gold standard for musculoskeletal imaging, but advancements in technology have made high-resolution diagnostic ultrasound the imaging modality of choice for rotator cuff injuries.
What makes high resolution ultrasound superior to MRI:

Most people take everyday mobility for granted until an injury occurs or pain sets in. Sometimes pain and reduced mobility seem to arise out of nowhere, with no apparent cause of onset. Regardless of whether your pain is caused by trauma or by something less obvious, tensegrity plays a key role.
Tensegrity refers to tensile integrity – a state where a system of individual components is held together under continuous elastic tension. In the human body, tensegrity is created by the myofascial system, the network of muscles and fascia that work together to produce, control, and guide forces, and to hold the body’s various organs and structures in place during movement.
Tensegrity can be disrupted when myofascial tissues are injured or damaged in some way. When that happens, nerves and blood vessels can become entrapped, preventing them from gliding among other structures and producing pain. At the same time, the elastic tension that governs joint alignment and controls movement becomes compromised, creating motor deficits that undermine mobility and stability.
Factors that disrupt myofascial tensegrity include:Many doctors do not understand the crucial role of the myofascial system in preventing pain syndromes, movement disorders, and disease. In fact, most medical doctors have no idea how to correct myofascial dysfunction or even recognize it as a factor. They simply treat pain symptoms with medications and eventually recommend surgery.
At NYDNRehab, we understand that the body’s systems work together as an integrated whole, and that treating pain is not enough to eliminate its source. We use dynamic high-resolution ultrasound to explore the myofascial system in real time. Ultrasound imaging lets us visualize muscles, fascia, nerves and other structures in motion, to identify places where tensegrity has been disrupted.
Once we identify the problem, we use the most advanced therapeutic approaches to restore myofascial integrity and promote tissue healing.
Identifying and treating underlying issues prior to beginning physical therapy is key to getting fast and effective results. Failure to pre-treat your condition can completely undermine your treatment protocol, and in some cases, your condition may even worsen.
At NYDNRehab, we use a broad range of regenerative technologies and integrative therapeutic approaches to resolve issues that can stand in the way of successful physical therapy. Our staff is certified in a diverse array of holistic treatment methodologies, and our one-on-one treatment sessions are personalized, based on your unique diagnostic profile.
Once we pre-treat your damaged tissues and eliminate compensation patterns, your shoulder complex will be ready for physical therapy.
The human body is made up of integrated parts and systems, designed to work in harmony. Today’s modern reductionist approach to medical treatment fails to acknowledge the integral relationship between structure and function, focusing on the locus of pain without considering its broader implications.
Most injuries involve multiple structures and tissue types, and pain is only a symptom that signals your brain to protect and heal the damaged tissues. It is not uncommon for an injury to stop hurting while damaged structures remain dysfunctional.
At NYDNRehab, our diagnostic process takes into account the interrelated nature of the body’s structures and systems, along with the unique anatomical characteristics of the individual patient. We use high resolution diagnostic ultrasound to visualize your injury dynamically, in real time, to determine whether structural (anatomical) changes are causing pain and dysfunction, or if dysfunction is causing structural changes.
Your ultrasound exam takes place on-site, on your first visit, where we examine multiple areas of the body in a single session – with no waiting for lab results!
The complexity of the shoulder region makes it difficult for practitioners to identify the exact source of shoulder pain and dysfunction. In many cases, multiple factors come into play. High resolution ultrasound imaging is an advanced and effective diagnostic tool, especially when coupled with new technologies that dramatically enhance visualization and facilitate shoulder rehabilitation.
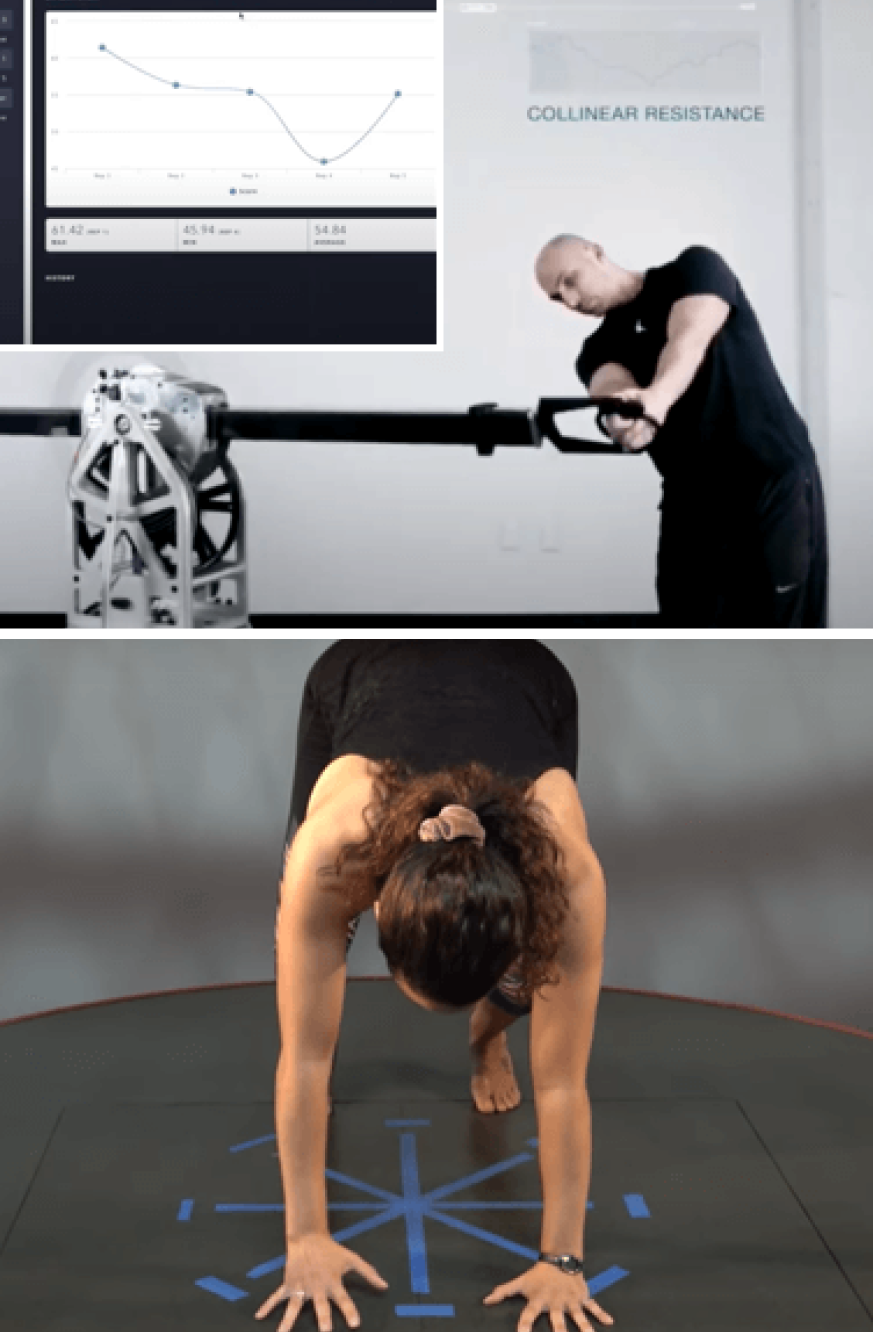
ShowMotion is an objective tool for joint movement analysis that uses motion tracking sensors, placed on the patient’s skin to collect data about movement quality. The patient performs a series of joint-specific movements, and the data is analyzed by ShowMotion’s proprietary software and displayed on a computer screen. The collected information provides valuable insights about inefficient movement patterns, compensation patterns, and improvements in movement in response to therapy, enabling practitioners to personalize rehabilitation.
ShowMotion is similar to gait /running analysis, but for the shoulder and scapular region. This cutting-edge technology can play a key role in postural restoration. ShowMotion can also contribute to athletic performance enhancement by measuring baseline joint kinematics and tracking the athlete’s progress in response to training.
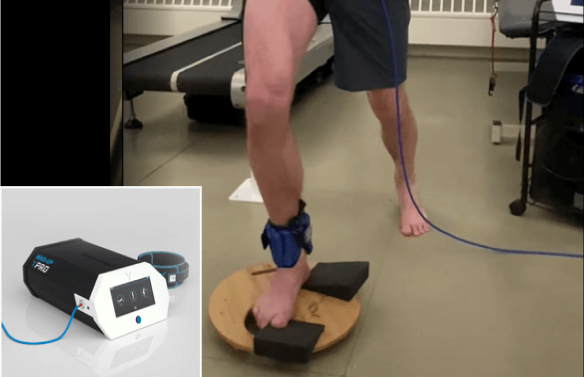
The Neuralign Shoulder Pacemaker is a shoulder rehabilitation device with a kinematic sensor activated by movement. The patient dynamically interacts with the device to stimulate efficient muscle recruitment patterns, enhance movement quality, and restore optimal muscle balance during rehabilitation. The sensor provides objective data that practitioners can use to support decision-making and personalize shoulder rehabilitation.
The Shoulder Pacemaker can be used to target several common conditions:
The Shoulder Pacemaker is also a cutting-edge tool for enhancing athletic performance in shoulder-intensive sports like swimming, tennis, baseball, and others.

The human body has its own innate healing mechanisms, but rotator cuff tendons sometimes need a nudge to accelerate the healing process. Regenerative technologies help to jump-start tendon healing by stimulating tissue repair at the cellular level. Our outpatient regenerative therapies expedite recovery with minimal discomfort for the patient.

SoftWave is a groundbreaking regenerative mechanotransduction technology that accelerates tissue healing. Its patented electro-hydraulic applicator delivers high-speed soundwaves that can penetrate up to six inches in depth. SoftWave’s defocused and linear focused shockwaves recruit maximum stem cells to the treatment site to promote healing. SoftWave’s wider and deeper penetration using defocused energy is a preferred treatment option for a broad spectrum of conditions, ranging from orthopedic injuries to pelvic health. SoftWave is the only unfocused shockwave technology currently available. According to recent research, SoftWave defocused waves combined with focused and radial shockwaves have maximum regenerative potential.
MyACT is a new type of focused shockwave technology that allows for deeper compression of the focused waves. Its higher frequency allows for precise neuro modulation under ultrasound guidance, with a special linear head for treating myofascial pain. MyACT transforms the mechanical energy of shockwaves into biochemical signals that precisely target damaged tissues. Most injuries involve more than one tissue type. When used together, our advanced shockwave technologies enable us to specifically target multiple tissue types with the most effective shockwave treatment.


Focused ESWT is used as a regenerative treatment for damaged tendon, muscle and bone tissue. This technology produces high frequency sound waves to stimulate the body’s own reparative mechanisms. It is especially effective for chronic degenerative tendon disorders and myofascial pain syndrome.
EMTT transmits high energy magnetic pulses to targeted tissues that synchronize with the body’s own magnetic fields, triggering a regenerative response. EMTT waves can penetrate deep tissues to target difficult-to-reach tendons, muscles, bones and nerves.


EPAT, sometimes called defocused shock wave therapy, is not a true shockwave. It uses mechanical pressure waves to enhance blood circulation, improving oxygen and nutrient delivery to muscle and fascia tissues, but has minimal regenerative properties.The mechanical properties of EPAT make it especially effective for fascial manipulation in combination with focused shockwaves. We combine EPAT with different types of shockwaves for holistic treatment, without additional cost to the patient.
HEIT delivers high-intensity magnetic pulses to peripheral nerve tissues, to stimulate neuroplasticity. We leverage this FDA-approved methodology to treat pain and regenerate nerve fibers, for enhanced motor control.


INDIBA is a form of TECAR therapy that helps to restore the ionic charge of damaged cells, for faster injury healing and rehabilitation.
NESA generates a low-frequency electrical current of intermittent and cyclical stimuli that soothes hypersensitized nerves and restores optimal signaling between the autonomic nervous system and the brain. We leverage this FDA-approved methodology to treat pain and regenerate nerve fibers, to enhance motor control.

Injection therapies use orthobiologic solutions that stimulate cellular repair by either nourishing or irritating the targeted cells. Dr. Kalika partners with an injection specialist, providing ultrasound guidance to ensure that the injected substances hit their mark, for maximum effectiveness.

PRP therapy uses a sample of the patient’s own whole blood, which is spun in a centrifuge to extract a high concentration of platelets. When injected into damaged tissues, PRP initiates tissue repair by releasing biologically active factors such as growth factors, cytokines, lysosomes and adhesion proteins. The injected solution stimulates the synthesis of new connective tissues and blood vessels. PRP can help to jump-start tendon healing in chronic injuries and accelerate repair in acute injuries.
Alpha 2 macroglobulin (A2M) is a naturally occurring blood plasma protein that acts as a carrier for numerous proteins and growth factors. As a protease inhibitor, A2M reduces inflammation in arthritic joints and helps to deactivate a variety of proteinases that typically degrade cartilage.
Prolotherapy uses a biologically neutral solution to irritate stubborn tissues, triggering the body’s innate healing mechanisms to grow new normal tendon, ligament and muscle fibers.
Shoulder injuries often involve fascial tissue that has become densified and/or formed adhesions, entrapping nerves and blood vessels, causing pain and restricting movement. Hydrodissection is a procedure where a saline solution is injected into densified fascia under ultrasound guidance. The solution works by separating fascial layers and freeing up entrapped nerves and blood vessels. We often use hydrodissection in conjunction with manual fascial manipulation.

SM neuromuscular electrical stimulation (NMES) dynamically interacts with the patient during therapeutic exercises, providing real-time sensory, auditory and visual biofeedback to the patient. This breakthrough technology helps patients to recalibrate muscle actions, to optimize joint function. SMNMES has helped numerous patients to avoid unnecessary shoulder, knee and ankle surgeries, even in complex scenarios.
During PENS treatment, filament-thin needles are inserted through the skin into muscle tissue adjacent to the targeted nerve. A low frequency electrical current is then delivered via the inserted needles to stimulate the dysfunctional nerve. PENS normalizes nerve activity, improves brain plasticity and optimizes muscle recruitment patterns. This therapy is so effective that patients typically need only 4-6 treatment sessions.
Abnormal scapular mechanics is the number one cause of rotator tendon overload. Scapular instability arises as a consequence of muscle weakness, inefficient muscle coordination patterns, poor posture, and muscle imbalances. Densified fascia and myofascial trigger points also contribute to scapular instability.
Dr. Kalika specializes in restoring scapular tensegrity using high resolution ultrasound, dynamic maneuvers, and Shomotion technology to enable panoramic views of the shoulder complex.
Specialized examination skills help to rule out:
Most rotator cuff tears do not require surgery, with the exception of full-thickness tears. Nevertheless, surgery is often recommended by doctors who do not understand the complexity of the shoulder joint and the many factors that contribute to scapular instability. Our holistic approach allows for diagnostic precision, enabling us to individualize shoulder therapy based on our findings.
Treatment approaches to restore scapular stability include shockwave therapy, prolotherapy injections, DNS, and Neuralign therapy.
At NYDNRehab, we treat the whole patient, not just your symptoms. We never use one-size-fits-all rehab protocols or antiquated recovery timelines. We believe that every injury is unique, and treatment should be based on a holistic approach that factors in the patient’s unique profile.
Once we have successfully pre-treated damaged tissues, we can begin one-on-one physical therapy to restore strength and stability, optimize mobility, and re-establish optimal neuromuscular pathways and muscle coordination patterns.
Every baby is born with internal software that governs the development of functional movement patterns during early childhood. Shortly after birth, a young infant begins to follow a developmental pathway that starts with head lifting and progresses through various stages to upright walking. But developmental movement patterns learned early in life are sometimes disrupted later on due to injury, repetitive overuse or disease.
DNS is a holistic treatment approach that taps into your primal developmental software to help restore efficient movement patterns and optimize pain-free shoulder function. Every joint in your body depends on local stabilizing muscles, tendons and ligaments, as well as coordination of both local and distal muscles, to maintain a neutral position of the humeral head in its socket. As a highly mobile joint, the shoulder relies heavily on both local and global stabilizers to assist in force transfer while protecting shoulder architecture.
The shoulder is a complex anatomical unit made up of 3 bones (scapula, clavicle and humerus), and four joints – sternoclavicular, acromioclavicular, scapulothoracic and glenohumeral. There are 17 muscles affecting the scapula, 5 muscles affecting the clavicle, and 10 ligaments holding the humeral head in its socket. To generate and transfer forces during physical activity, optimal shoulder function requires all of these structures to work together in coordinated patterns.
Many trainers, therapists and chiropractors spend their time trying to restore the function of individual muscles, rather than focusing on coordinated movements with the shoulder in a properly centrated position. Dynamic neuromuscular stabilization helps to optimize shoulder function by correcting joint misalignment and restoring coordinated muscle recruitment patterns that have been lost over time.
Conventional treatment for rotator cuff injuries often involves rest, anti-inflammatory drugs, NSAIDs, physical therapy exercises, steroid injections and surgery. However, conventional approaches often fall short of restoring full function, especially for athletes.
Advancements in technology are changing the game in rehabilitative medicine, enabling us to accelerate healing and restore performance at an unprecedented pace. The clinic at NYDNRehab features some of the most advanced therapeutic equipment currently available, and rarely found in private clinics.
Your rotator cuff therapy may include the use of high-tech equipment:

Originally developed to rehabilitate injured soldiers, this multifaceted system gives us a broad range of tools for assessment, feedback and performance enhancement. Dr. Kalka has integrated his own unique selection of technologies to optimize the ways in which C.A.R.E.N helps patients to achieve their goals.



Independent peer-reviewed research relevant to this treatment approach.