Medicine is constantly discovering new insights into human anatomy and physiology, and trochanteric hip bursitis pain is no exception. Hip bursitis goes by many names, including greater trochanteric pain syndrome, lateral hip pain and gluteus medius tendinopathy, but they all describe the same pain in your hip. New research has given us a paradigm shift on hip pain that significantly improves treatment outcomes.
Chronic lateral hip pain is a common complaint of women over the age of 50, with 23.5% reporting either unilateral or bilateral hip pain. Lateral hip pain occurs four times more often in women than in men.
The trochanter bursa is a fluid-filled sac surrounding the surface of the greater trochanter. An inflamed bursa is rarely the primary source of hip pain, but rather a reaction of the bursa tissue to degeneration of the gluteus minimus or medius tendons. Despite the name “bursitis,” the causative mechanism is really a primary tendinopathy and not an inflamed bursa.
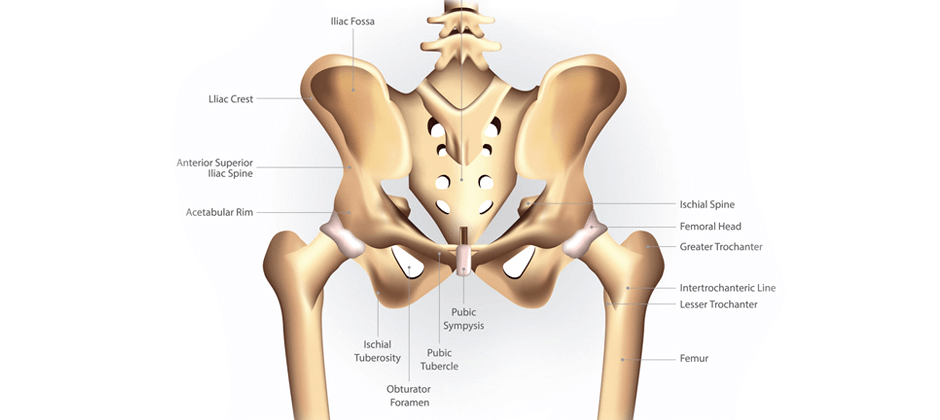
The hip is a complex joint, located in the midst of numerous neuromuscular and anatomical structures, including the lumbar spine and sacroiliac joint, any of which can evoke lateral hip pain. Yet the greater trochanteric bursa has been historically blamed for lateral hip pain, and patients are often misdiagnosed with bursitis when their pain stems from another source.
The following studies suggest alternative causes of this type of hip pain:
When lateral hip pain is universally assumed to be caused by bursitis, all treatments are geared to reducing inflammation. Pain and inflammation are first managed with NSAIDs, followed by cortisone injections, and then on to surgical interventions. Yet physical therapy is rarely considered as treatment for lateral hip pain, even though evidence strongly suggests that bursitis is rarely the primary cause.
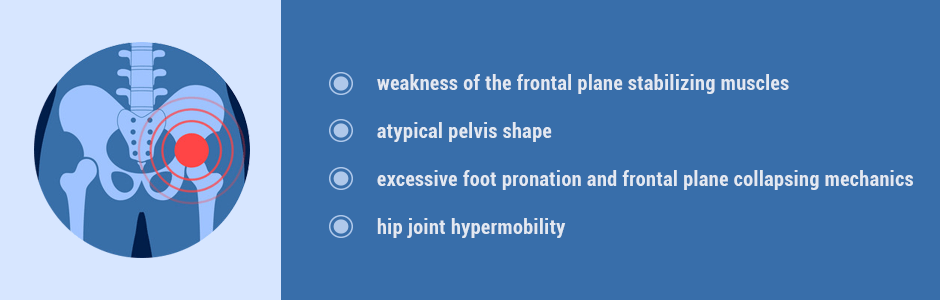
The primary cause of tendon deterioration is thought to be overload of the medial gluteal tendons due to:

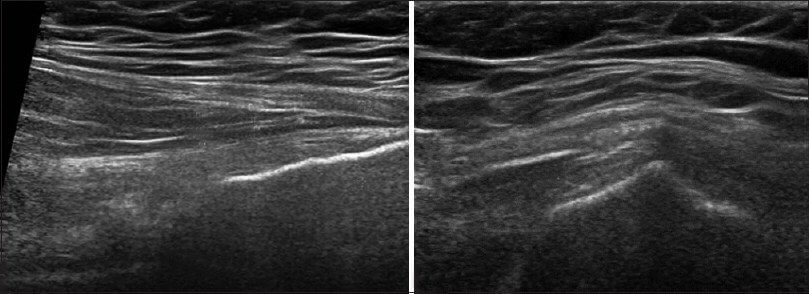
A clinical exam and diagnostic ultrasound imaging can help your therapist pinpoint the exact location and cause of your hip and groin pain.
Ultrasound enables you and your therapist to view the hip and groin region in real time, while in motion. In addition to ultrasound, video gait analysis can help us identify faulty movement mechanics that contribute to hip and groin pain. Once the exact cause is determined, an effective treatment plan can be initiated.
Please explore more advanced diagnostic option unavailable anywhere else:

The sports medicine professionals at NYDNRehab understand human movement science and how mechanical deficiencies can lead to structural pain. We conduct a comprehensive physical exam, ultrasound imaging and 3D motion and gait analysis testing for motor deficiencies, to get to the bottom of your lateral hip pain.
NYDNRehab is committed to not just treating your pain, but to resolving it by getting to the source. Our advanced treatment strategies are cutting edge, geared to getting you back on your feet and physically active again. Call NYDNRehab today, and find out why we are the leading specialists for lateral hip pain in NYC.
Get all the benefits of physical therapy and chiropractic care via safe and effective online sessions, all from the privacy and convenience of your home, office or hotel room. Never miss a session, and keep moving toward your physical therapy goals.
Extracorporeal shockwave therapy(ESWT) , has proven to be the most effective and non-invasive modality for treating bursitis, with a 93% success rate, according to research. While ESWT can relieve pain and regenerate gluteal tendons, it does not improve mechanical issues, motor control or gait.
Gait-specific physical therapy must be undertaken to improve:
At NYDNRehab we use the most advanced hip physical therapy approaches to improve all related movement deficiencies. Our clinic features the most advanced technologies available in the US to retrain the lower kinetic chain. Our Computer Assisted Rehabilitation Environment (C.A.R.E.N.) is the very first technology to provide instantaneous movement feedback based on pressure, forces, kinematics, and artificial intelligence algorithms, enabling brain-muscle retraining.
Our testing protocol includes:
Combined lumbopelvic hip stability test using DLEST methodology with C.A.R.E.N., our computer assisted rehab environment
Hip joint stability test using DLEST methodology with C.A.R.E.N.
3D star excursion banner test (SEBT) for assessing the involvement of the hip joint and muscles in postural stability
3D gait or running analysis
3D kinematic joint angle analysis during a squat, lunge, drop jump and pelvis on hip rotation
Rehabilitative ultrasonography for viewing intrinsic hip stabilizing muscle activation patterns
Dr. Lev Kalika is a world-recognized expert in musculoskeletal medicine. with 20+ years of clinical experience in diagnostic musculoskeletal ultrasonography, rehabilitative sports medicine and conservative orthopedics. In addition to operating his clinical practice in Manhattan, he regularly publishes peer-reviewed research on ultrasound-guided therapies and procedures. He serves as a peer reviewer for Springer Nature.
Dr. Kalika is an esteemed member of multiple professional organizations, including: