March 25, 2025
Achilles tendon injuries are common among athletic and fit populations, especially in running and jumping sports. For decades, the standard of care for Achilles tendinopathy has centered on progressive loading and pain management. But recent advancements in technology are dramatically disrupting conventional treatment approaches and ushering in a new era of regenerative therapies for tendon injuries.
Learn how platelet rich plasma (PRP) and shockwave therapy stack up as holistic therapeutic approaches for Achilles tendinopathy, and how high-resolution ultrasonography changes the game for diagnosis and treatment.
Tendons are made up mostly of collagen (65-80%) and elastin (1-2%) fibers embedded in an extracellular matrix of water and glycoproteins. Collagen fibers are the basic structural units of tendons, bound together by a thin sheath of connective tissue called endotenon. The fibers are grouped together in bundles, and multiple bundles make up the tendon itself.
Tendon fibers are organized in parallel, and also cross over each other to form spirals, creating a complex architecture designed to withstand longitudinal, transversal and rotational forces. A tendon’s main job is to transmit muscle forces to the bone, making joint movement possible. The Achilles tendon also stores and releases elastic energy as it lengthens and shortens during physical activity, contributing to forward and upward propulsion.
The Achilles tendon is the widest and strongest tendon in your body, and Achilles injuries typically fall under one of two categories – cumulative microtrauma to the tendon fibers from chronic repetitive overuse and training errors, or acute tendon ruptures in the course of physical activity. In sedentary populations, Achilles tendinopathy can arise from disuse and atrophy of the muscles and tendon.
Males and females are equally at risk for Achilles tendinopathy, with the peak age for incidence between 40-59 years. Because the main body of the tendon has limited vascularity, tendon injuries can be slow to heal. If left untreated, the tendon can begin to degenerate, developing abnormalities in its molecular structure, composition and cell matrix that cause pain and functional decline.
Tendinopathy is essentially a failed healing response, where the tendon fibers become haphazardly arranged in irregular patterns. At the same time, an increase in the non-collagenous matrix and calcification of the tendon may occur, along with increased cross-sectional area, reduced tendon stiffness, and loss of viscoelastic properties.
Symptoms of Achilles tendinopathy include pain, inflammation and reduced function during physical activity. While the condition is sometimes called tendinitis or tendinosis, tendon experts agree that tendinopathy is the most accurate and appropriate terminology. The term tendinitis is considered a misnomer because it implies certain biological processes and inflammatory activity that may not be present in the injured tendon.
Achilles tendinopathy most often occurs at the tendon’s mid-portion – accounting for about two-thirds of cases – but it can also occur where the tendon inserts at the calcaneus (heel bone). Insertional tendinopathy and mid-portion (noninsertional) tendinopathy each have distinct features and require unique treatment strategies.
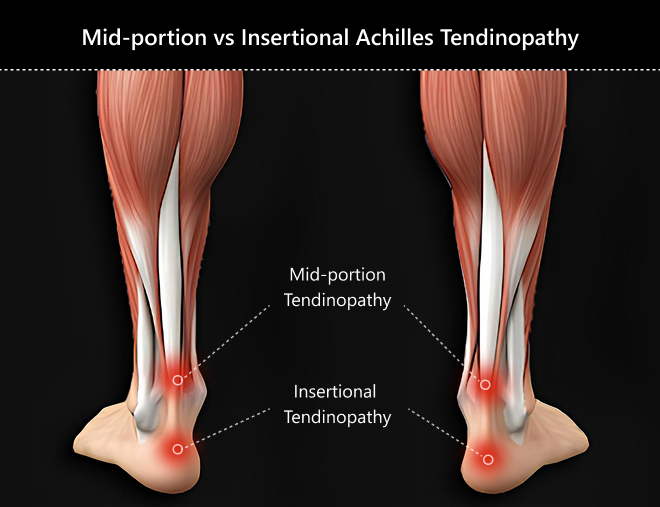 Mid-portion Achilles tendinopathy occurs 2 to 6 cm proximal to the insertion of the tendon on the calcaneus. Patients often report pain during physical activity and morning stiffness. Pain often has a gradual onset, sometimes intermittent or worsening over time. The affected area is usually tender to palpation, with palpable thickening.
Mid-portion Achilles tendinopathy occurs 2 to 6 cm proximal to the insertion of the tendon on the calcaneus. Patients often report pain during physical activity and morning stiffness. Pain often has a gradual onset, sometimes intermittent or worsening over time. The affected area is usually tender to palpation, with palpable thickening.
Insertional Achilles tendinopathy occurs at the site of insertion at the calcaneus. It shares similar symptoms to mid-portion tendinopathy, but the pain is localized to the tendon insertion. Of the two categories, insertional tendinopathy is typically more severe, and may be accompanied by bone spurs, calcifications, and enlargement of the calcaneal bursa.
Achilles tendinopathy is often diagnosed based on the patient’s history and clinical exam. The location of tendinopathy (mid-portion vs insertional) is most often determined by palpation and patient feedback, with tenderness and thickening being key indicators.
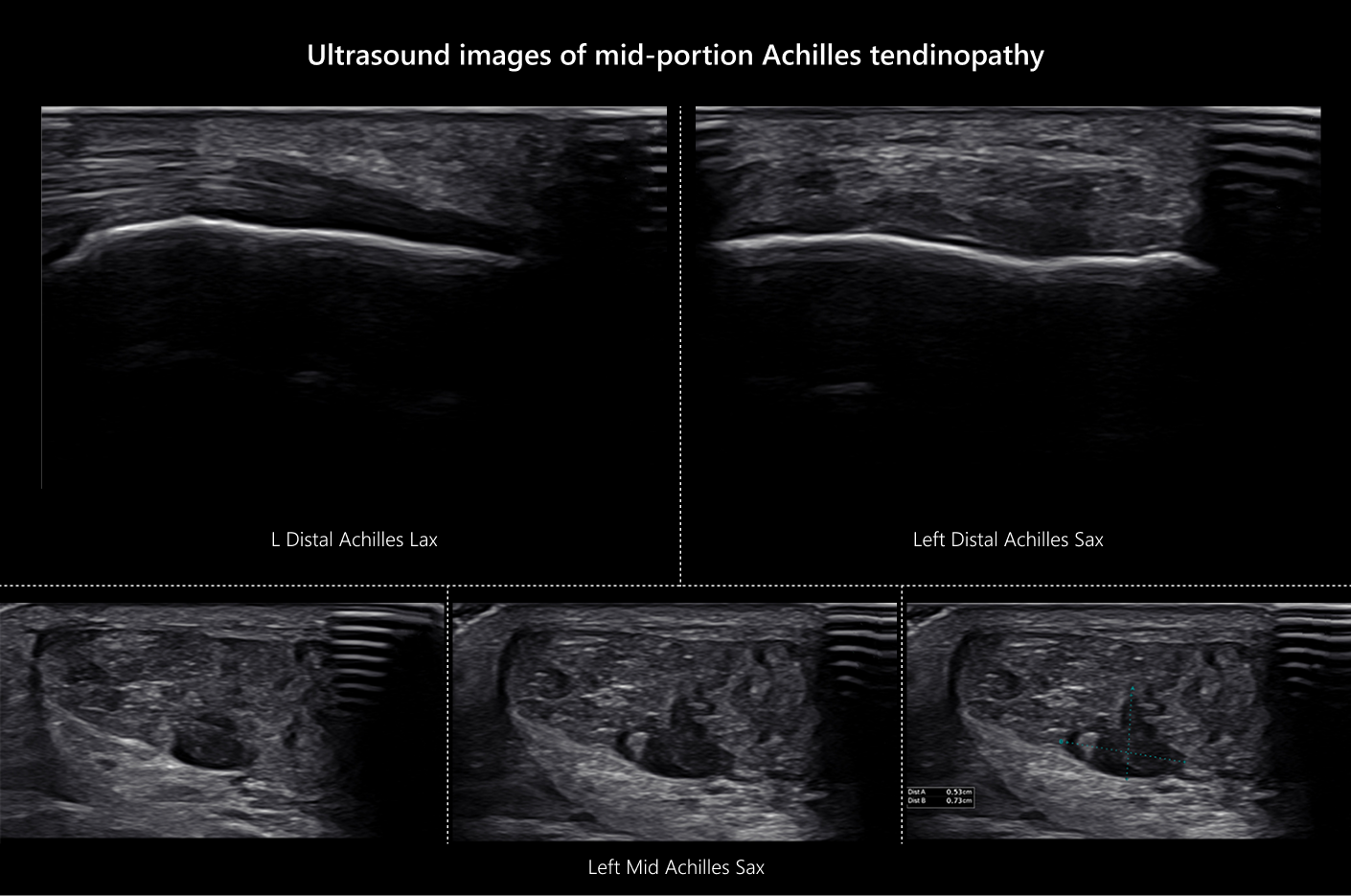
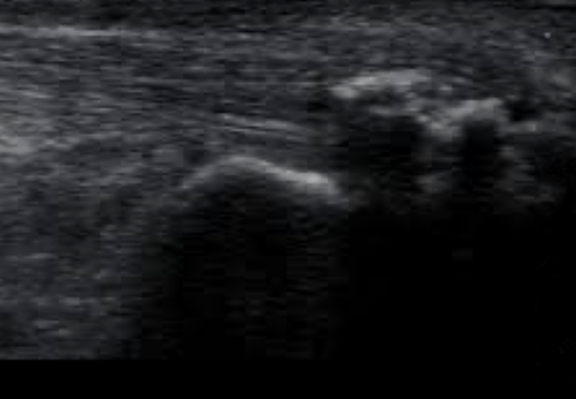
Imaging with Xray or MRI may be of some use, but imaging with high-resolution ultrasonography has multiple advantages, providing dynamic images in real time.
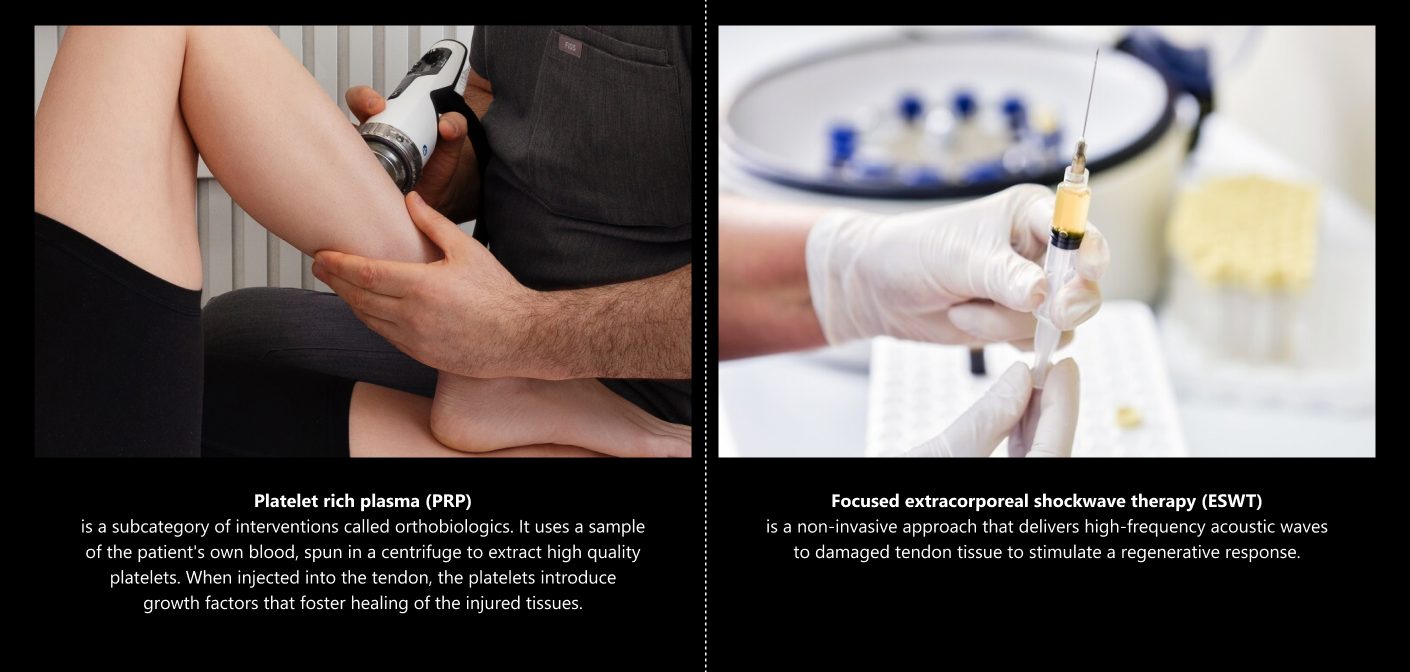
Platelet rich plasma (PRP) is a subcategory of interventions called orthobiologics. It uses a sample of the patient’s own blood, spun in a centrifuge to extract high quality platelets. When injected into the tendon, the platelets introduce growth factors that foster healing of the injured tissues.
PRP promotes Achilles tendon healing by:
Focused extracorporeal shockwave therapy (ESWT) is a non-invasive approach that delivers high-frequency acoustic waves to damaged tendon tissue to stimulate a regenerative response.
Shockwave therapy promotes tendon healing by:
A recent review of randomized controlled trials concluded that adding ESWT to a tendon loading program resulted in improved patient perception of their recovery from mid-portion Achilles tendinopathy, but not from insertional Achilles tendinopathy.
Shockwaves are often used in conjunction with progressive eccentric loading and other treatment modalities to optimize tissue healing. A multimodal approach to Achilles tendinopathy that includes progressive eccentric loading, PRP injections and focused and radial shockwave therapy is likely to accelerate and optimize patient healing.
For athletes, appropriate sport-specific training is key to preventing Achilles tendinopathy. Stretching and plantar strengthening exercises that target the Achilles can help prevent tendon ruptures in impact sports. Strengthening the posterior kinetic chain is recommended, along with optimizing tibiotalar and subtalar joint mobility.
For non-athletic populations, remaining physically active with exercises like walking that load the lower kinetic chain can go a long way toward preventing Achilles tendon injuries.
Additionally, a number of medications have been associated with tendinopathy, including:
If you are being treated with prescription medications, consult with your physician before beginning or intensifying your exercise program, to ensure that your meds do not increase your risk of Achilles tendon injury.
If left untreated, Achilles tendinopathy can continue to degenerate over time, impacting your mobility and quality of life. It’s never too late to rehabilitate your Achilles tendon, even if your injury happened years ago. The tendon specialists at NYDNRehab use the latest technologies and regenerative therapies to treat tendon injuries. We visualize your damaged tissues on-site, using the highest-resolution ultrasonography to diagnose your condition, track your progress, and guide regenerative procedures.
Don’t let an injured Achilles keep you from enjoying your favorite sports and activities. Contact NYDNRehab today, and get advanced treatment so you can get back out there!
Frairia, Roberto, and Laura Berta. “Biological effects of extracorporeal shock waves on fibroblasts. A review.” Muscles, ligaments and tendons journal 1.4 (2011): 138.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3666484/
Neph, Alyssa, et al. “Role of mechanical loading for platelet-rich plasma-treated Achilles tendinopathy.” Current sports medicine reports 19.6 (2020): 209-216.
Role of mechanical loading for platelet-rich plasma-treated Achilles tendinopathy
Paantjens, Marc A., et al. “Extracorporeal shockwave therapy for mid-portion and insertional Achilles tendinopathy: a systematic review of randomized controlled trials.” Sports Medicine-Openi> 8.1 (2022): 68.
Extracorporeal shockwave therapy for mid-portion and insertional Achilles tendinopathy: a systematic review of randomized controlled trials
von Rickenbach, Kristian J., et al. “Achilles tendinopathy: evaluation, rehabilitation, and prevention.” Current sports medicine reports 20.6 (2021): 327-334.
https://journals.lww.com/acsm-csmr/fulltext/Achilles_Tendinopathy__Evaluation_Rehabilitation
Dr. Lev Kalika is a world-recognized expert in musculoskeletal medicine. with 20+ years of clinical experience in diagnostic musculoskeletal ultrasonography, rehabilitative sports medicine and conservative orthopedics. In addition to operating his clinical practice in Manhattan, he regularly publishes peer-reviewed research on ultrasound-guided therapies and procedures. He serves as a peer reviewer for Springer Nature.
Dr. Kalika is an esteemed member of multiple professional organizations, including: