Many conventional physical therapists take a one-size-fits-all approach to patient care, using antiquated timelines and cookie cutter exercises that fail to fully rehabilitate knee injuries and restore optimal movement.
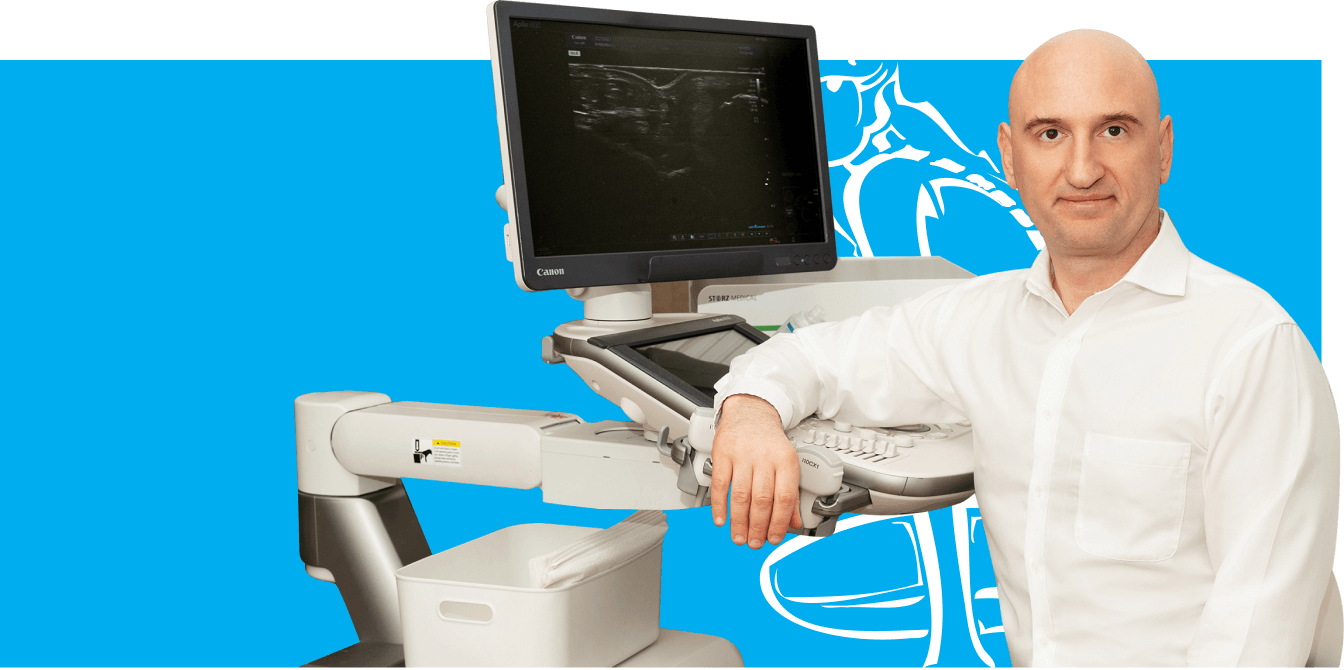
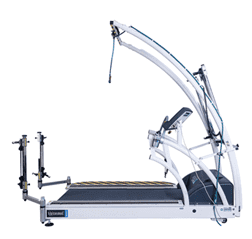
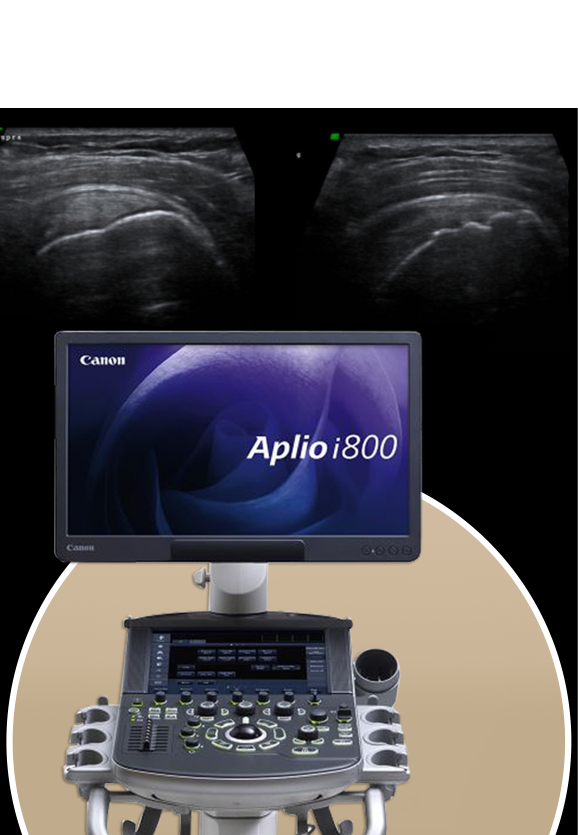
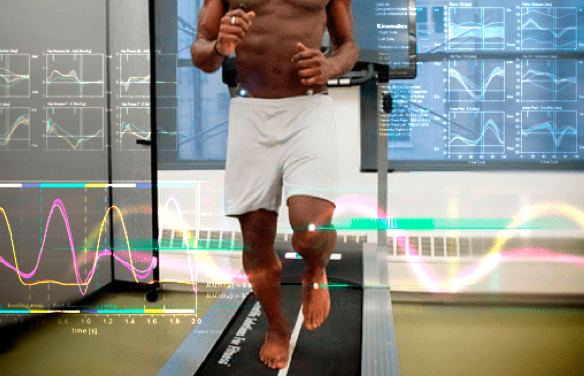
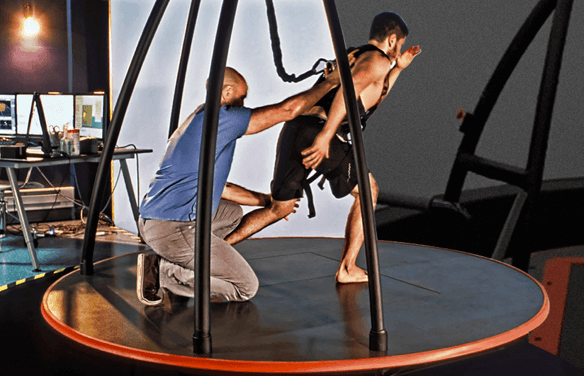
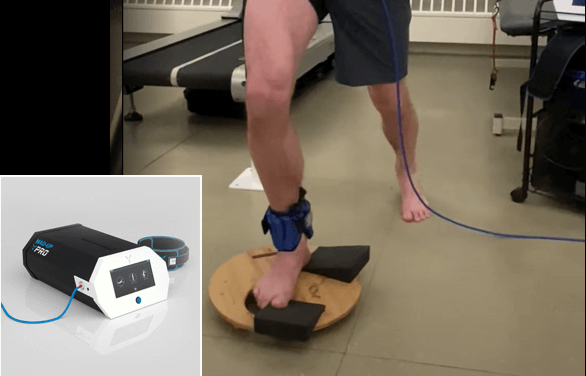
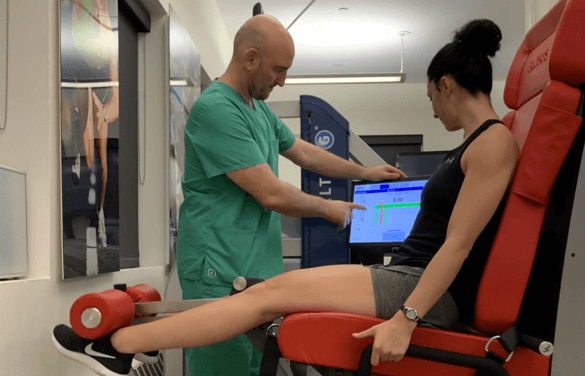
At NYDNRehab, we take an individualized approach to every patient and every condition. Using advanced technologies, we are able to accurately diagnose and measure individual parameters for joint angles, force loads, muscle firing patterns and gait. We then design personalized treatment programs based on collected data, measuring progress along the way to ensure full recovery.
Our experience combining innovative treatment methods with advanced technologies makes NYDNRehab the number one choice for physical therapy, chiropractic care and rehabilitation in NYC.
We use FDA approved methodologies to successfully treat a broad range of conditions. Our patients include elite athletes, runners and ballet dancers who come to us for rehab and performance enhancement.



























 Dr. Yuri Brosgol
Dr. Yuri Brosgol  Dr. Michael Goynatsky
Dr. Michael Goynatsky  Dr. Daniela Escudero
Dr. Daniela Escudero  Dr. Michelle Agyakwah
Dr. Michelle Agyakwah  Dr. Tatyana Kapustina
Dr. Tatyana Kapustina