August 28, 2025

Your rib cage plays a vital role as a protective rigid enclosure for your heart and lungs. It also functions as an attachment site for your respiratory muscles, including your intercostal muscles and diaphragm, and provides structural support for your upper body.
From a biomechanical standpoint, your ribcage serves to stabilize your thoracic spine during movement, and helps to regulate your breathing aparatus. In addition, all the fascial chains from your lower and upper limbs converge at the rib cage, as do the fascia that connect to your visceral organs.
Because your rib cage interacts with your thoracic spine during movement and expands during respiration, injuries to the rib cage can be quite painful and debilitating, causing pain during physical activity and interfering with breathing. Physical therapy can help you get to the bottom of your rib cage pain and resolve it.
Your rib cage is made up of 12 sets of ribs:
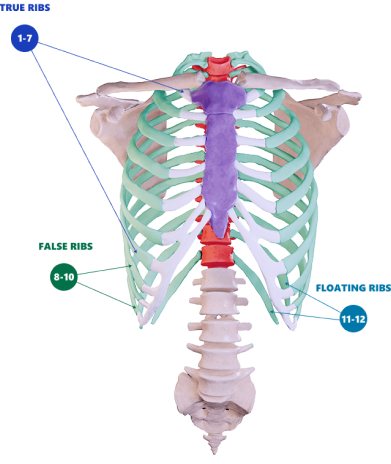
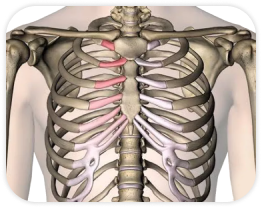
Ribs 1-7: The uppermost sets of ribs are often called “true ribs” because they attach to both the front and back sides of your body. On the posterior side, your true ribs join with your thoracic vertebrae at the costovertebral and costotransverse joints. On the anterior (front) side, they attach to your sternum by way of the costal cartilage.
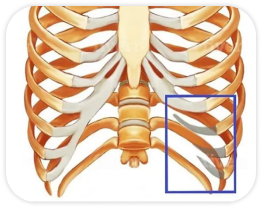
Ribs 8-10: Beneath the “true ribs” lie the “false ribs.” Ribs 8-10 attach to the thoracic spine in the same manner as ribs 1-7, but they do not attach directly to the sternum. Instead, each false rib attaches to the cartilage of the rib above it.
Ribs 11 and 12: The lower ribs are called “floating ribs” because they only attach to their corresponding vertebra on the posterior side; in front, they are not attached, so they simply float.
Each rib has a costal groove on the inside of the rib along the lower border to allow for the passage of intercostal veins, arteries and nerves.
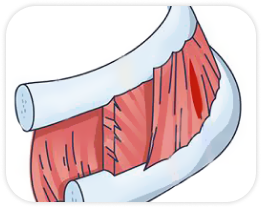
The spaces between the ribs are occupied by two thin layers of intercostal muscles that run at right angles to one another. The external intercostals form the top layer and act at the rib cage as you breathe in. The internal muscles form the inside layer and contract as you exhale.
Trigger points and fascia densification and adhesions are very common in the rib cage, and those are often a greater source of pain than the muscles themselves. In addition, a complex network of arteries, veins and nerves pass through the thorax, and those can easily become entrapped by fascia adhesions, inhibiting movement and causing pain.
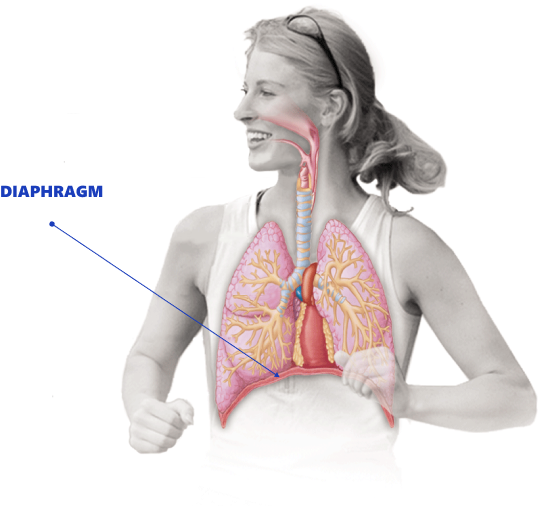
The diaphragm is most often thought of as a respiratory muscle, but it also plays an important role in spinal stability. The left side of the diaphragm especially contributes to maintenance and regulation of posture, while the right side plays a larger role in respiration. The entire diaphragm provides rib cage stability and spinal support by regulating intrathoracic and intra abdominal pressure.
Fascia is a thin dense sheet of connective tissue that encases bundles of muscle fibers so they can glide independently of other muscles and move freely among bones, nerves and vital organs. Fascia has multiple sensory neurons that help your body’s systems communicate with one another. Because fascia is highly innervated, it can generate significant pain when injured.
During respiration, your thoracic and abdominal fascia interact in coordinated patterns to regulate breathing according to oxygen demand. The patterns vary with respiratory rate, and with thoracic and abdominal movements
To function at its best, fascia needs to remain supple and elastic. Repetitive motion activities and overtraining can cause overuse injuries to the fascia that make it stiff and tight. Stiff fascia can often be the root cause of rib fascia pain, interfering with your breathing apparatus and limiting your trunk range of motion.
Sometimes adhesions can develop in your fascia, causing it to stick rather than glide, often entrapping nerves and blood vessels in the process. Fascial adhesions in one area of your body can affect structures in other areas.
Thoracic fascia adhesions can affect mobility and stability throughout your upper body. In the chest and ribs, internal diseases very often present as musculoskeletal symptoms, transmitted via the fascia.
Rib cage pain can arise from injury to any of the muscles, bones, nerves or joints within the thoracic cage region. Some of the most common causes of rib cage pain stem from sports and physical activity.
Stress Injuries to the Rib Bones
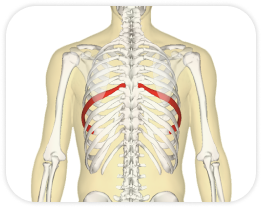
Rib bone stress injuries most commonly occur in athletes who play sports like golf, swimming, running, rowing and throwing sports. They are especially common in elite rowers, with female rowers at greater risk. Rib stress injuries most frequently occur in ribs 4 to 8.
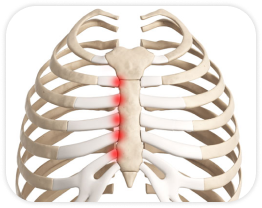
Costochondritis
Costochondritis is a condition most often seen in ribs 2 to 5 that manifests as left side rib pain, accounting for up to 30% of emergency chest pain visits. It occurs most often in adults over 40, and more frequently in women. Costochondritis is associated with repetitive trunk and arm movements, chest wall trauma, and chronic coughing. Its symptoms are tenderness in the joints and cartilage of the affected ribs. Prior to diagnosing costochondritis, a thorough exam and chest x-ray should be done to rule out cardiac issues.
Tietze Syndrome
Tietze syndrome (TS) is a rare condition that mostly affects adults between the ages of 20-40. TS is similar to costochondritis in that it involves joint tenderness, but it most often affects joints 2 and 3 and is marked by inflammation.
Slipping Rib Syndrome
Slipping rib syndrome (SRS) is a somewhat uncommon condition that affects the cartilaginous attachments of the false ribs. The cartilage may become subluxated, causing pain and possible nerve impingement. The syndrome is more common in female athletes in sports like running, rowing, swimming and lacrosse, and often manifests as debilitating lower rib cage pain.
Posterior Rib Joint Dysfunction
This condition is frequently described as “subluxation,” but there is little evidence to support that notion. Thoracic pain at the back of the rib cage is most commonly seen in rowers and swimmers. The condition responds well to manual therapy.
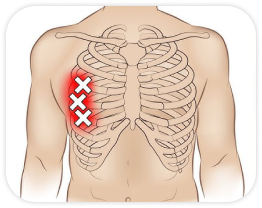
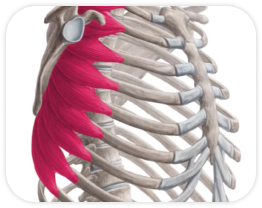
Serratus Anterior Strain
Athletic strain of the serratus anterior muscle is most commonly seen in rowers and athletes who play overhead sports like golf, tennis and baseball. Symptoms are pain on the side of the ribcage.
Intercostal Muscle Strain
Up to 50% of rib cage pain is caused by strain of the intercostal muscles that run between the ribs. Sports that require repetitive upper body movements like tennis, rowing and baseball increase the risk of intercostal strain.
Transient Upper Abdominal Pain
Pain at the lower side of the rib cage, often called a side stitch, occurs most often in young athletes during sports like swimming and running. Pain can sometimes radiate from the lower rib cage to the shoulder.
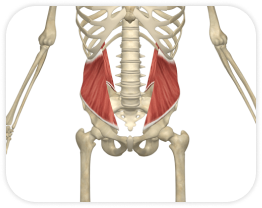
Oblique Muscle Strain
The internal and external oblique muscles are responsible for trunk rotation, and they can become strained during explosive rotation activities like pitching a baseball or swinging a bat. Oblique strains are most often felt as side rib pain in lower ribs 9 through 12, and may increase with deep breathing or coughing.
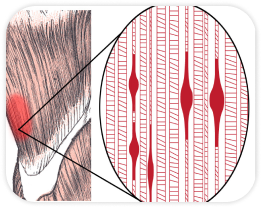
Myofascial Trigger Points
Trigger points are tight nodules of contracted fascia or muscle tissue that can cause both local and referred pain. They often occur from overtraining, and can affect both superficial and deep tissues. Superficial trigger points can be palpated from the skin’s surface and are easily treated with manual therapy or dry needling. Deep tissue trigger points can only be detected with imaging, and can be treated with ultrasound guided dry needling. Trigger points can affect the muscles that surround and support the rib cage, causing pain and limiting range of motion.
Referred Visceral Pain
Pain that stems from the visceral organs such as the liver, pancreas, GI tract, heart or lungs can sometimes manifest as rib cage pain, transmitted via the fascia. Unlike musculoskeletal pain, visceral pain does not diminish or increase with movement, change in position or palpation.
Because there are so many things that can cause rib cage pain, a thorough exam is needed to rule out visceral sources of pain. A thorough health history and physical exam can help determine the underlying cause of rib cage pain.
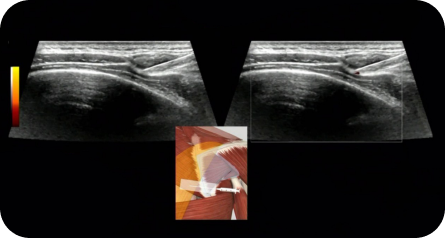
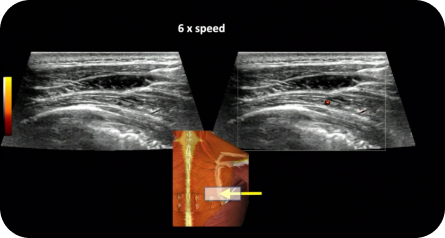
At NYDNRehab, we use diagnostic ultrasonography to view the structures of the thorax and rib cage in motion, in real time. When combined with feedback from the patient, ultrasound imaging can help us pinpoint the exact location and source of pain, enabling us to decide on the most effective treatment solutions.
While Xray and MRI can show bone pathologies like cancer, the dynamic capabilities of high resolution diagnostic ultrasound make it far more useful in cases such as:
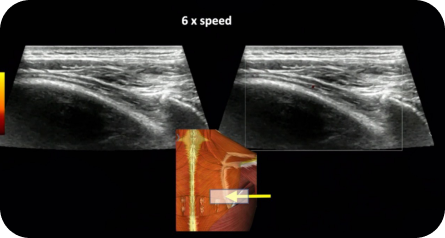
Unlike MRI or Xray, high resolution diagnostic ultrasound lets us examine multiple areas in a single visit:
Another important diagnostic tool for rib cage disorders is the thoracic ring approach, an evidence-based approach described by world renowned researchers, Diane and LJ Lee that examines the mobility and range of motion of the thorax and rib cage, Poor thoracic mobility is associated with low back pain and cervical spine pain.
Dr. Kalika is certified in thoracic ring methodology, and uses it in conjunction with diagnostic ultrasonography to visualize rib movement and view the intercostal and thoracic nerves with the thorax in motion.
Imaging of the scapula using high-resolution ultrasound is an important tool for observing how the scapula moves relative to the humeral head of the shoulder joint. Accurate interpretation requires a skilled clinician with a comprehensive knowledge of human anatomy. Combining scapular ultrasound with ShowMotion technology provides substantial information for comprehensive shoulder rehabilitation.
Scapular imaging is especially useful for patients with rotator cuff tears, joint hypermobility syndrome (JHS), or Ehlers-Danlos syndrome (EDS) whose joints are prone to excessive movements and instability. In such cases, the connective tissues surrounding the shoulder joint tend to be lax and weak, causing poor joint stability and increasing the risk of shoulder subluxation/dislocation.
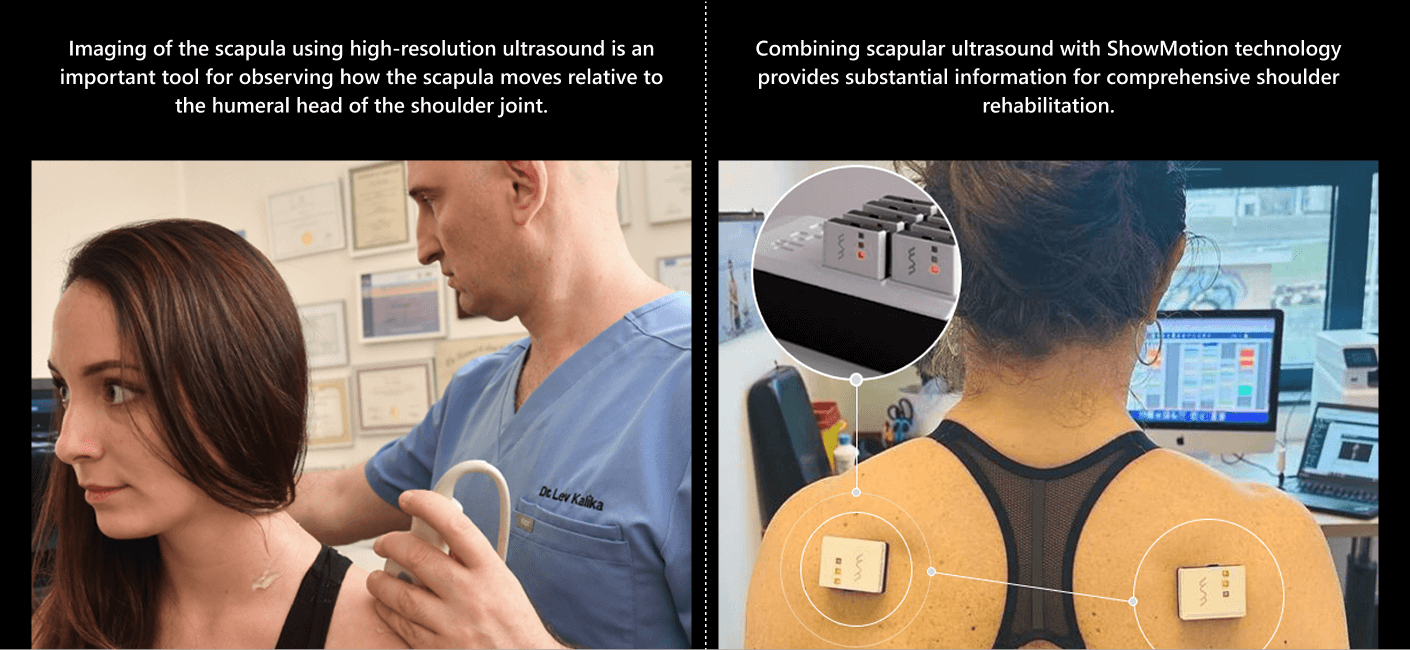
The scapula compensates for shoulder instability by acting as a stable base for positioning the glenoid fossa, to optimize positioning of the humeral head. Dynamic scapular stabilization requires well-coordinated muscle activation patterns, especially of the rotator, deltoid, trapezius and rhomboid muscles. Scapular dysfunction can increase strain on the rotator cuff and labrum, contributing to pain and instability.
Dynamic scapular imaging lets us observe the complex interactions of the shoulder girdle kinetic chain, to pinpoint issues such as deficiencies in muscle activation, glenohumeral joint subluxation, and capsular laxity that contribute to shoulder instability. For patients with rotator cuff tears , JHS/EDS patients, scapular ultrasound can be a game-changer, ensuring they receive proper rehabilitation that enhances stability after a shoulder dislocation.
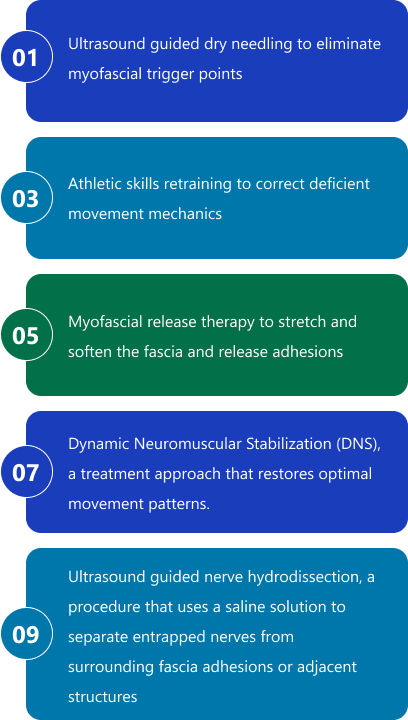
Physical therapy can help you get to the source of your rib cage pain and restore healthy pain-free function. Treatment options may include:
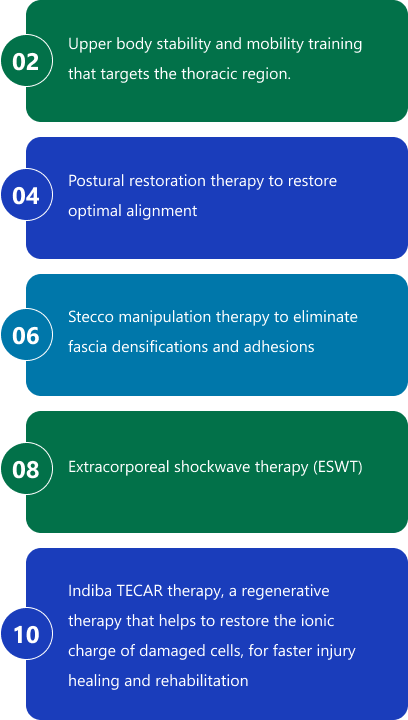
Rib cage pain requires specialized treatment from a skilled practitioner. At NYDNRehab, we work with thoracic cage pain using specialized soft tissue manipulation of the myofascial structures of the rib cage, to release adhesions and increase mobility of the ribs and thoracic spine.
You don’t have to live with rib cage pain. Contact NYDNRehab today, and get rid of your rib cage pain so you can get back to doing the things you love.
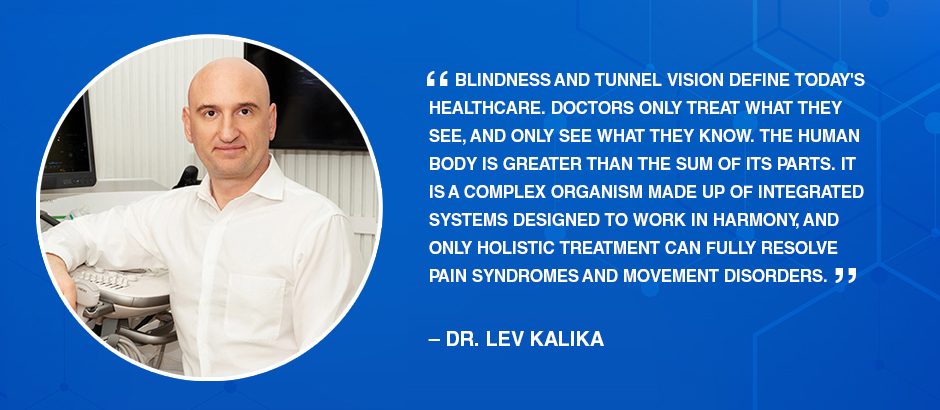
Dr. Lev Kalika is a world-recognized expert in musculoskeletal medicine. with 20+ years of clinical experience in diagnostic musculoskeletal ultrasonography, rehabilitative sports medicine and conservative orthopedics. In addition to operating his clinical practice in Manhattan, he regularly publishes peer-reviewed research on ultrasound-guided therapies and procedures. He serves as a peer reviewer for Springer Nature.
Dr. Kalika is an esteemed member of multiple professional organizations, including: