August 27, 2025
 Low back, neck and shoulder pain get a lot of attention in the healthcare world due to their frequent incidence, but very little mention is made of the thoracic spine. Yet thoracic mobility and stability play an important role in human movement, and dysfunction in the thoracic spine is a chief contributor to pain in other regions of the spine and body.
Low back, neck and shoulder pain get a lot of attention in the healthcare world due to their frequent incidence, but very little mention is made of the thoracic spine. Yet thoracic mobility and stability play an important role in human movement, and dysfunction in the thoracic spine is a chief contributor to pain in other regions of the spine and body.
Learn about the thoracic spine, its role in sports and everyday movement, and how improving thoracic mobility can impact your overall health and physical performance.
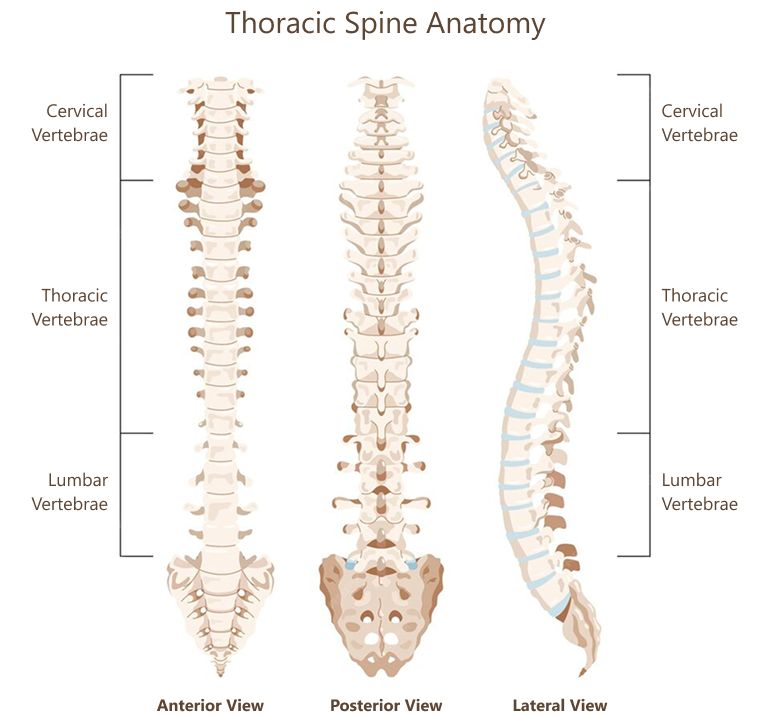
The thoracic spine is made up of 12 vertebrae, numbered T1-T12, that bridge the cervical spine and the lumbar spine. The thoracic vertebrae are separated by flexible cartilage discs that provide cushioning and shock absorption, allowing for spinal rotation and flexion.The thoracic spine is the longest segment of the spinal column, and arguably the most important in terms of function.
Functions of the thoracic spine include:
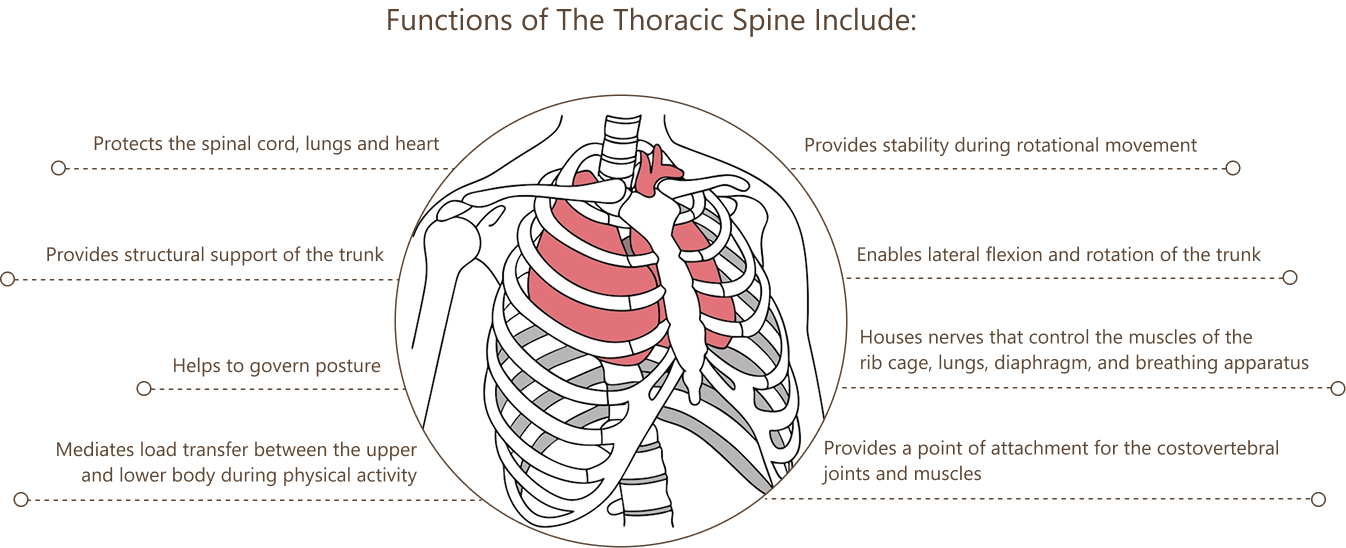
The rib cage is connected to the thoracic spine by the costovertebral joints, attaching all but the bottom two ribs to the spine. The thoracic spine and rib cage work together to stabilize the chest and abdomen, provide a bony framework that protects the heart and lungs, and help to regulate breathing mechanics. A radiate ligament encases the costovertebral joints, providing stability and restricting rib cage movement to only slight gliding actions.
The thoracic architecture is uniquely designed to enable trunk rotation, which is essential to all dynamic movement. Walking, running and most sports rely on trunk rotation to help maintain balance, transfer force loads, generate momentum, and enable arm and shoulder movement. Many sports like tennis, golf, baseball and hockey rely on trunk rotation to generate force when striking a ball or puck.
The thoracic spine serves as a key transitional point for distributing force loads between the head, shoulders and pelvis. It provides stability for rotational movements via its connection with the rib cage, and the surrounding muscles and fascia. When there is insufficient trunk rotation during dynamic movement, rotational stress is transferred to other structures such as the neck and shoulders, lower back, pelvis, hips, and lower extremities.
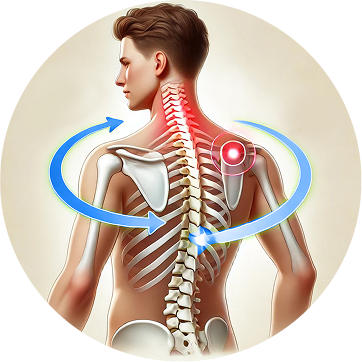
People who suffer from pain in the neck, shoulders and low back often have limited trunk rotation, and it can even cause issues like tennis elbow and golfer’s elbow. Reduced thoracic mobility can cause issues with the shoulder girdle, such as scapular dyskinesis and subacromial impingement.
Stiffness in the thoracic spine can limit your ability to breathe deeply by restricting movement of the lungs and diaphragm. Shallow breathing can have far-reaching repercussions for metabolic health, cellular function, tissue healing, and posture. Reduced oxygen flow can limit the ability of your cellular mitochondria to manufacture ATP, the energy molecule, resulting in fatigue and reduced physical performance.
Thoracic mobility is closely related to scapular stability – the ability of the muscles surrounding the scapula to hold the shoulder blade in position and control its movement. The shoulder blade plays a critical role in shoulder function, posture, and upper body movement. The loss of scapular stability is called scapular dyskinesis, where the scapula moves abnormally, especially when the arm is raised and lowered.
Good thoracic mobility enables proper scapular positioning and movement. At the same time, good scapular stability supports efficient thoracic mobility. When one or the other is deficient, it can affect shoulder function, posture, and upper body performance. In cases of scapular dyskinesis, the thoracic spine and ribs may compensate for excess shoulder and scapular movement by becoming stiff and immobile – a protective mechanism of the muscles
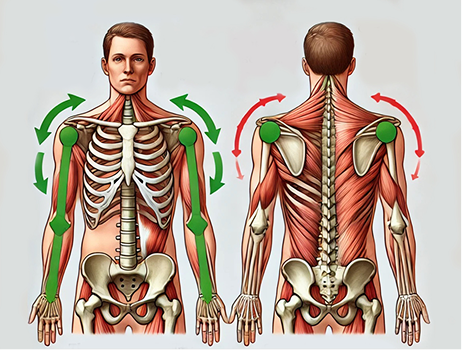
Good thoracic mobility enables proper scapular positioning and movement. At the same time, good scapular stability supports efficient thoracic mobility. When one or the other is deficient, it can affect shoulder function, posture, and upper body performance. In cases of scapular dyskinesis, the thoracic spine and ribs may compensate for excess shoulder and scapular movement by becoming stiff and immobile – a protective mechanism of the muscles
A stiff thoracic spine reduces the range of motion for overhead movements like reaching or throwing, forcing the scapula to overcompensate. This can increase stress on the rotator cuff or neck muscles and cause tension in the fascia, preventing the scapula from gliding smoothly along the rib cage. Strong scapular stabilizers enhance the thoracic spine’s ability to move by providing a solid base for dynamic actions.
The interdependent nature of the thoracic spine and scapula demonstrates how pain and dysfunction in one region of the body can cause loss of mobility in another area, disrupting the entire kinetic chain. The body’s biomechanical interdependence underscores the need for complex therapeutic approaches that are personalized and comprehensive.
Treating only the locus of pain without addressing other structures further along the kinetic chain can create additional compensatory changes that fail to improve functional mobility.
Imaging of the scapula using high-resolution ultrasound is an important tool for observing how the scapula moves relative to the humeral head of the shoulder joint. Accurate interpretation requires a skilled clinician with a comprehensive knowledge of human anatomy. Combining scapular ultrasound with ShowMotion technology provides substantial information for comprehensive shoulder rehabilitation.
Scapular imaging is especially useful for patients with rotator cuff tears, joint hypermobility syndrome (JHS), or Ehlers-Danlos syndrome (EDS) whose joints are prone to excessive movements and instability. In such cases, the connective tissues surrounding the shoulder joint tend to be lax and weak, causing poor joint stability and increasing the risk of shoulder subluxation/dislocation.
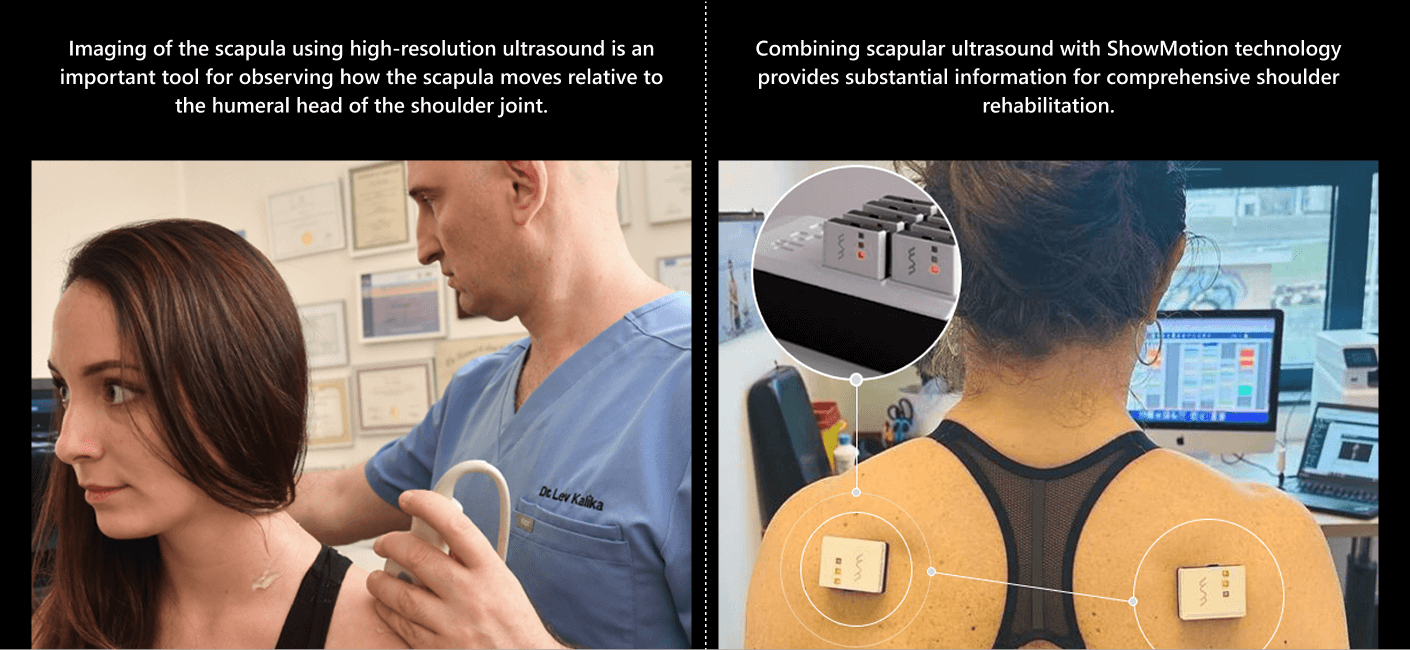
The scapula compensates for shoulder instability by acting as a stable base for positioning the glenoid fossa, to optimize positioning of the humeral head. Dynamic scapular stabilization requires well-coordinated muscle activation patterns, especially of the rotator, deltoid, trapezius and rhomboid muscles. Scapular dysfunction can increase strain on the rotator cuff and labrum, contributing to pain and instability.
Dynamic scapular imaging lets us observe the complex interactions of the shoulder girdle kinetic chain, to pinpoint issues such as deficiencies in muscle activation, glenohumeral joint subluxation, and capsular laxity that contribute to shoulder instability. For patients with rotator cuff tears , JHS/EDS patients, scapular ultrasound can be a game-changer, ensuring they receive proper rehabilitation that enhances stability after a shoulder dislocation.
The sympathetic nervous system (SNS) originates in the thoracic and lumbar regions of the spinal cord, extending from the first thoracic vertebra to the second or third lumbar vertebra, depending on individual anatomy.
A part of the autonomic nervous system, the sympathetic nervous system is often referred to as the “fight or flight” system, because it governs the body’s reactions to stressful or threatening scenarios. In such scenarios, the SNS releases norepinephrine from postganglionic neurons, sparking a cascade of physiological reactions.
Physiological changes triggered by the SNS include:
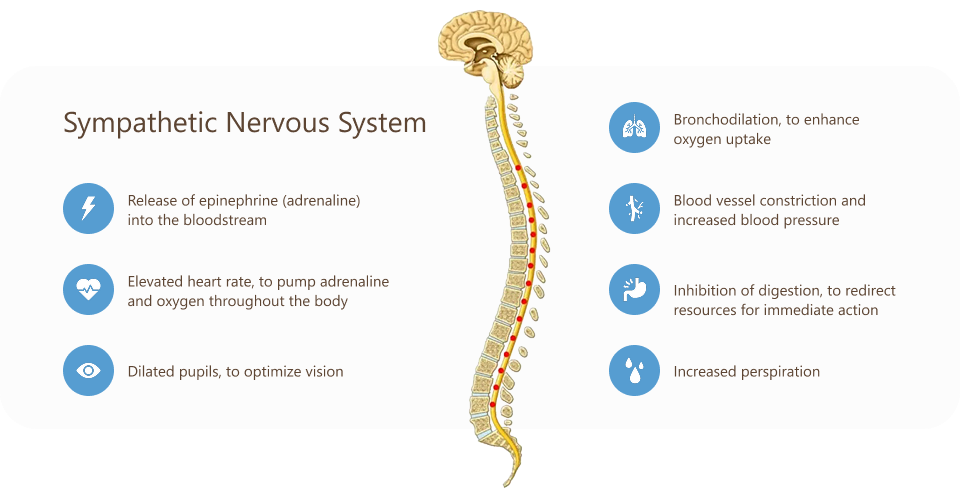
Mobility of the thoracic spine directly impacts the sympathetic nervous system due to the arrangement of nerve fibers of the sympathetic chain that run alongside the thoracic vertebrae. Restrictions in thoracic rotation can stimulate increased sympathetic activity, inducing a state of chronic stress and causing nerves to become hypersensitized. By contrast, optimal thoracic mobility can help to downregulate the SNS and promote a better balance between the sympathetic and parasympathetic nervous systems
Tensegrity refers to a state of tensile integrity, where a system of individual components is held together under continuous elastic tension. In the human body, tensegrity is created by the myofascial system, where fascia’s elastic tension counterbalances muscle contraction and force production. Tensegrity holds vital organs in place during movement, creates symmetry, and enables the body’s systems to move and work in harmony.
Fascia is a type of connective tissue that encases and connects muscles and vital organs throughout the body. Fascia works together with muscles to control and guide movement, generate and transfer force loads, facilitate breathing, and provide a slippery ecosystem that enables nerves, blood vessels and other structures to glide without friction during movement.
The thoracolumbar fascia (TLF) consists of multiple layers of crosshatched collagen fibres, creating a girdling structure that separates the paraspinal muscles from the muscles of the posterior abdominal wall. The TLF contains nociceptive free nerve endings that are thought to contribute to low back pain.
When injured, the TLF can become densified and sticky, losing its elastic properties and reducing the ability of fascial layers to slide. Damaged fascia can cause reduced thoracic mobility, spasticity, and increased tension in the lower thoracic and lumbar spine. Nerve endings can become hyper-activated, triggering sensitization, local inflammation and pain, and inhibiting muscle action.
Thoracic mobility promotes proper organ function, especially of the heart, lungs and breathing apparatus, but also of the pelvic organs. The relationship between the thoracic spine and pelvis merits attention, because improper breathing can cause pelvic organ prolapse if the pelvic bowl is not properly pressurized.
Intra abdominal pressure (IAP) is generated by the diaphragm as it flattens out to allow more air into the lungs. However, if the thoracic spine is tight, rib movement is restricted, making it difficult to fully inflate the lungs, and limiting diaphragm function.
When the thoracic spine curves forward, it increases resting pressure on the pelvic floor while reducing rib mobility.
Over time, poor posture from too much sitting can impact core and pelvic strength and stability. The transverse abdominis muscle of the deep core is directly connected to the thoracic fascia. Weakened muscles and limited thoracic mobility can cause various types of pelvic dysfunction, such as bladder incontinence, pelvic pain, constipation and diastasis recti during pregnancy.
The iliopsoas muscle, a powerful hip flexor that provides stability for the hip and lower back, originates at the twelfth vertebra of the thoracic spine. The hip flexors become tight with excessive sitting, creating poor posture and contributing to pelvic dysfunction. Because of the thoracic spine’s relationship to the pelvis, it is important to address thoracic mobility when treating pelvic floor disorders,
Poor thoracic rotation can affect the position and function of the shoulder blades, leading to scapular instability that affects posture and performance. To compensate for poor thoracic rotation, muscles of the neck, shoulders and back need to work harder. A stiff thoracic spine can cause shoulder impingement, and may contribute to rotator cuff pain.
Reduced thoracic mobility affects posture, causing stress on joints, muscles and fascia throughout the body. A forward head position, rounded shoulders and exaggerated low back arch are all associated with reduced thoracic mobility. When the thorax does not rotate well, the lumbar spine is forced to rotate, potentially causing lumbar disc compression and low back pain.
Factors that contribute to reduced thoracic mobility include:
Thoracic mobility can be improved with exercises and stretches that rotate the middle spine through its full range of motion, and that flex the trunk laterally (bending to the side).
Movement efficiency is key to physical performance and pain-free mobility. A comprehensive biomechanical analysis can help to pinpoint inefficient movement patterns and identify their causes. At NYDNRehab, we use advanced technologies for data-driven results, enabling us to accurately assess movement parameters and measure patient progress. If you’re tired of feeling stiff and achy, contact us today, and let us help you get moving again!
Erbes, Nicole A., et al. “Movement impairments in women with and without urinary urgency/frequency.” The Journal of Women’s & Pelvic Health Physical Therapy 45.4 (2021): 164-173.
Movement impairments in women with and without urinary urgency/frequency
Hunter, Donald J., et al. “Relationship between shoulder impingement syndrome and thoracic posture.” Physical therapy 100.4 (2020): 677-686.
Relationship between shoulder impingement syndrome and thoracic posture
Mellin, Guy. “Decreased joint and spinal mobility associated with low back pain in young adults.” Clinical Spine Surgery 3.3 (1990): 238-243
Decreased joint and spinal mobility associated with low back pain in young adults
Wang, Hao, et al. “Effects of trunk posture on cardiovascular and autonomic nervous systems: A pilot study.” Frontiers in Physiology 13 (2022): 1009806.
Effects of trunk posture on cardiovascular and autonomic nervous systems: A pilot study
Welbeck, A. N., et al. “Examining the link between thoracic rotation and scapular dyskinesis and shoulder pain amongst college swimmers.” Physical Therapy in Sport 40 (2019): 78-84.
Examining the link between thoracic rotation and scapular dyskinesis and shoulder pain amongst college swimmers
Dr. Lev Kalika is a world-recognized expert in musculoskeletal medicine. with 20+ years of clinical experience in diagnostic musculoskeletal ultrasonography, rehabilitative sports medicine and conservative orthopedics. In addition to operating his clinical practice in Manhattan, he regularly publishes peer-reviewed research on ultrasound-guided therapies and procedures. He serves as a peer reviewer for Springer Nature.
Dr. Kalika is an esteemed member of multiple professional organizations, including: