Pudendal neuropathy is a pain syndrome that affects both males and females, children and adults. In some patients it is thought to be caused by congenital anomalies in the pathway of the pudendal nerve. The condition is often made worse by excessive sitting.
While pudendal neuropathy is often treated with surgery, there are a number of highly successful alternative treatment options that pose much lower risk to the patient, with better long-term outcomes.
The pudendal nerve originates at the posterior pelvic wall, and is made up of fibers from nerve roots of the sacral vertebrae S2, S3 and S4. It is a mixed nerve with sensory, motor, and autonomic properties.
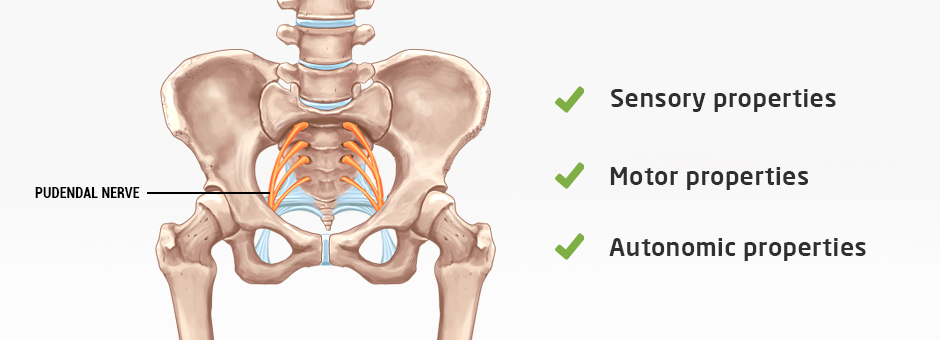
Sensory properties are responsible for innervating both male and female external genitals, as well as the anus, perineum and anal canal.
Motor properties innervate certain pelvic muscles, along with the urethral and external anal sphincters.
Autonomic properties control the inhibition and release of secretions.
Injury to the pudendal nerve or inflammation of surrounding tissues can lead to dysfunction of the bowels, bladder and reproductive organs.
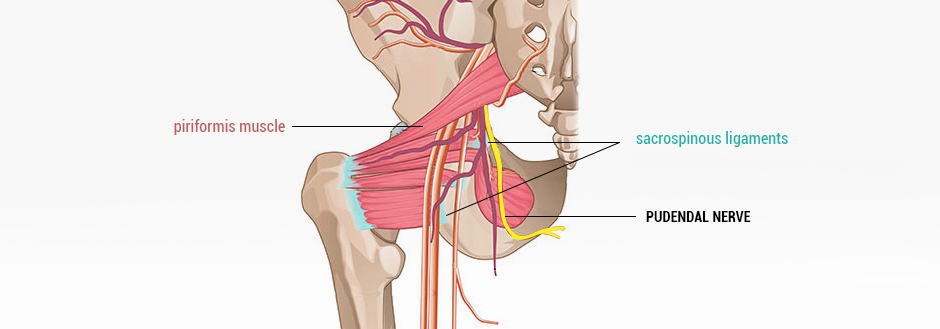
From the pelvic wall, the pudendal nerve travels behind the piriformis muscle and threads between the sacrotuberous and sacrospinous ligaments, which are sometimes responsible for impinging the nerve. From there, it travels through the pudendal canal, where it splits into the perineal nerve, the dorsal nerve of the penis or clitoris, and the inferior rectal nerve.
The structure and pathway of the pudendal nerve can vary from one patient to the next, making it imperative to seek help from an experienced professional who can make an accurate diagnosis based on your unique condition.
Pudendal neuropathy has been attributed to repetitive overuse of the pelvic floor muscles that causes cumulative microtrauma to the nerve. Over time, the condition can lead to structural remodeling of the ischial spine and sacrum. Symptoms have a gradual onset that intensifies with further damage if the condition is left untreated.
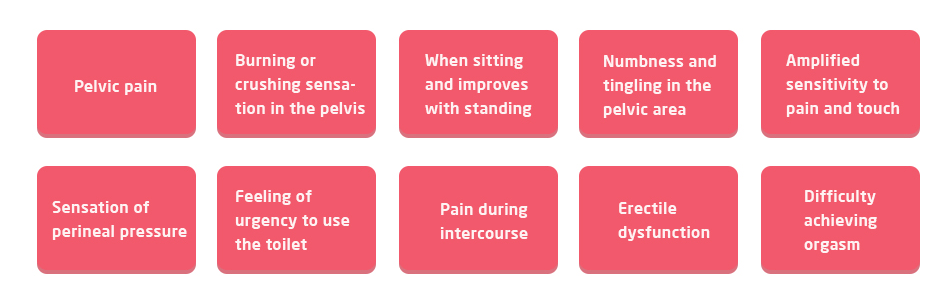
Peripheral neuropathy symptoms include:
Burning or crushing sensation in the pelvis
Pain that is worse when sitting and improves with standing
Numbness and tingling in the pelvic area
Amplified sensitivity to pain and touch
Sensation of perineal pressure, like you are retaining a golf ball
Feeling of urgency to use the toilet
Pain during intercourse
Erectile dysfunction
Difficulty achieving orgasm
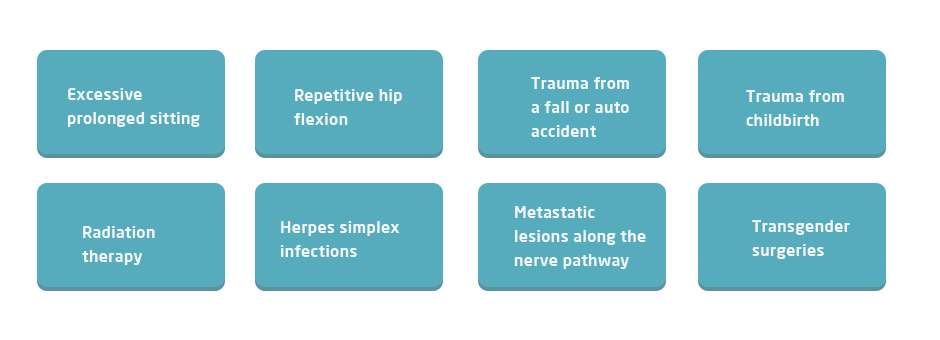
Common causes of pudendal neuropathy include:
Excessive prolonged sitting
Repetitive hip flexion during sports and exercise like running and cycling
Acute trauma from a fall or auto accident, or from pelvic surgery
Trauma from childbirth or sexual assault
Radiation therapy for prostate, rectal or gynecological cancers
Herpes simplex infections
Metastatic lesions along the nerve pathway
Transgender surgeries
Patients complaining of chronic pelvic pain are often treated by end-organ specialists, such as urologists, gynecologists, and colorectal surgeons. Many patients suffer for years, going from one specialist to the next in hopes of finding a lasting solution. Pain medications and surgeries are often the norm, putting patients at risk for opioid addiction.
In the realm of physical therapy, conventional treatment has centered on intrapelvic physical therapy via the vagina or rectum, and guided injections into the vicinity of the pudendal nerve. However, the evidence for intrapelvic physical therapy is very low, and intrapelvic nerve blocks have little research to support them.
Extracorporeal Shock Wave Therapy (ESWT)
Recent research shows that weekly ESWT treatments for chronic pelvic pain significantly reduce pain, improve urinary function, and enhance overall quality of life.
Ultrasound Guided Dry Needling
A new 2020 study conducted by Dr. Lev Kalika and a colleague found ultrasound guided dry needling to be highly effective for relieving pelvic pain and dysfunction caused by myofascial trigger points.
Cognitive Behavioral Therapy (CBT)
Pain is perceived by your brain, and physical pain is influenced by your thoughts and behaviors. CBT can help to alter the emotions, thoughts, and behaviors associated with pain, and can improve coping strategies. CBT helps patients recontextualize pain and discomfort, thereby changing the brain’s physiological response to pain.
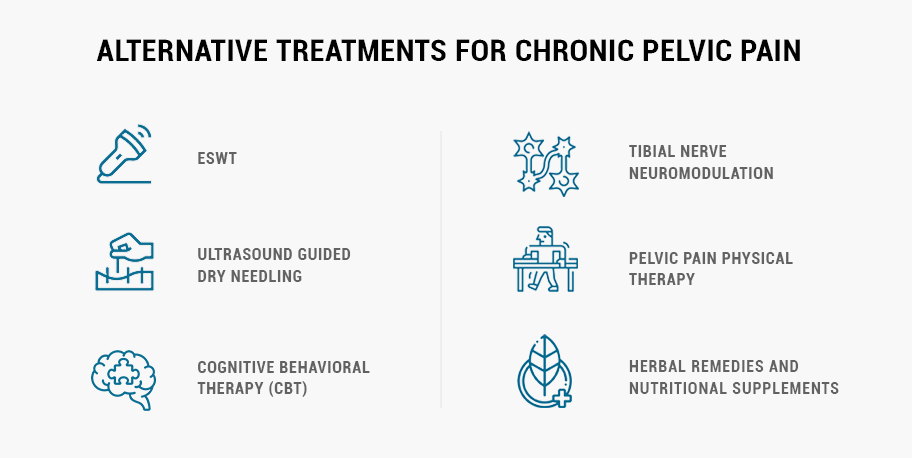
Tibial Nerve Neuromodulation
Percutaneous Tibial Nerve Stimulation (PTNS) is a conservative non-surgical treatment that uses a low electrical current to stimulate the nerves responsible for bladder and pelvic floor function.
Pelvic Pain Physical Therapy
Physical therapy can help restore balanced muscle tone and realign your spine and pelvis to alleviate pressure on the pudendal nerve and improve the overall integrity of the pelvic floor.
Herbal Remedies and Nutritional Supplements
Certain natural plant products and nutritional supplements are well-known for their nerve-calming properties, with minimal negative side effects. Herbal supplements can be applied topically, or used as vaginal or rectal suppositories. Common herbal remedies and supplements for pudendal neuropathy include:
Saint John’s Wort
Skullcap
Valerian root
Willow
Motherwort
Cayenne
Alpha-lipoic acid.
Acetyl-L-carnitine
Pelvic pain and pudendal neuropathy can be successfully treated with alternative, non-invasive or minimally invasive treatment options, so long as the practitioner has ample knowledge and experience. Dr. Lev Kalika has over 13 years of experience treating pelvic pain and dysfunction using a combination of focused and radial shock wave therapy, and ultrasound guided dry needling.
At NYDNRehab, we never use a one-size-fits all approach to treating pelvic pain and pudendal neuropathy. Our pelvic floor treatment protocols are custom designed for the individual patient, and our one-on-one approach ensures that you receive all the attention you need to successfully resolve your condition.
If you are ready to take a holistic alternative approach to pelvic pain, contact NYDNRehab today, and get rid of pelvic pain for good so you can get back to doing the things you love.
Resources
Dr. Lev Kalika is a world-recognized expert in musculoskeletal medicine. with 20+ years of clinical experience in diagnostic musculoskeletal ultrasonography, rehabilitative sports medicine and conservative orthopedics. In addition to operating his clinical practice in Manhattan, he regularly publishes peer-reviewed research on ultrasound-guided therapies and procedures. He serves as a peer reviewer for Springer Nature.
Dr. Kalika is an esteemed member of multiple professional organizations, including: