July 1, 2025
 Whether necessary or elective, abdominal surgery comes with multiple risks ranging from mild discomfort to life-threatening severity. One undesirable but common side effect of abdominal procedures is the formation of scar tissue and adhesions, affecting up to 90 percent of patients after abdominal surgery. However, many doctors, physios, and chiropractors are hasty to assume the presence of scar tissue and adhesions without objective evidence, leading patients down a path of mistreatment that can do more harm than good.
Whether necessary or elective, abdominal surgery comes with multiple risks ranging from mild discomfort to life-threatening severity. One undesirable but common side effect of abdominal procedures is the formation of scar tissue and adhesions, affecting up to 90 percent of patients after abdominal surgery. However, many doctors, physios, and chiropractors are hasty to assume the presence of scar tissue and adhesions without objective evidence, leading patients down a path of mistreatment that can do more harm than good.
Learn about the formation of abdominal scar tissue post-surgery, the health risks it poses, the best imaging modality for detection, and advanced non-invasive interventions for treating abdominal scarring and adhesions.
Scar tissue is the end result of soft tissue healing after surgery or trauma, where collagen fibers form to seal the wound and restore structural integrity. Unlike bone tissue that repairs itself with the same substance, soft tissues are mended with a fibrous matrix of collagenous tissue that is denser and less elastic than the original tissue. Scar tissue has a different structure and color, and lacks the full functionality of the injured tissues.
Scar tissue formation occurs in three phases:
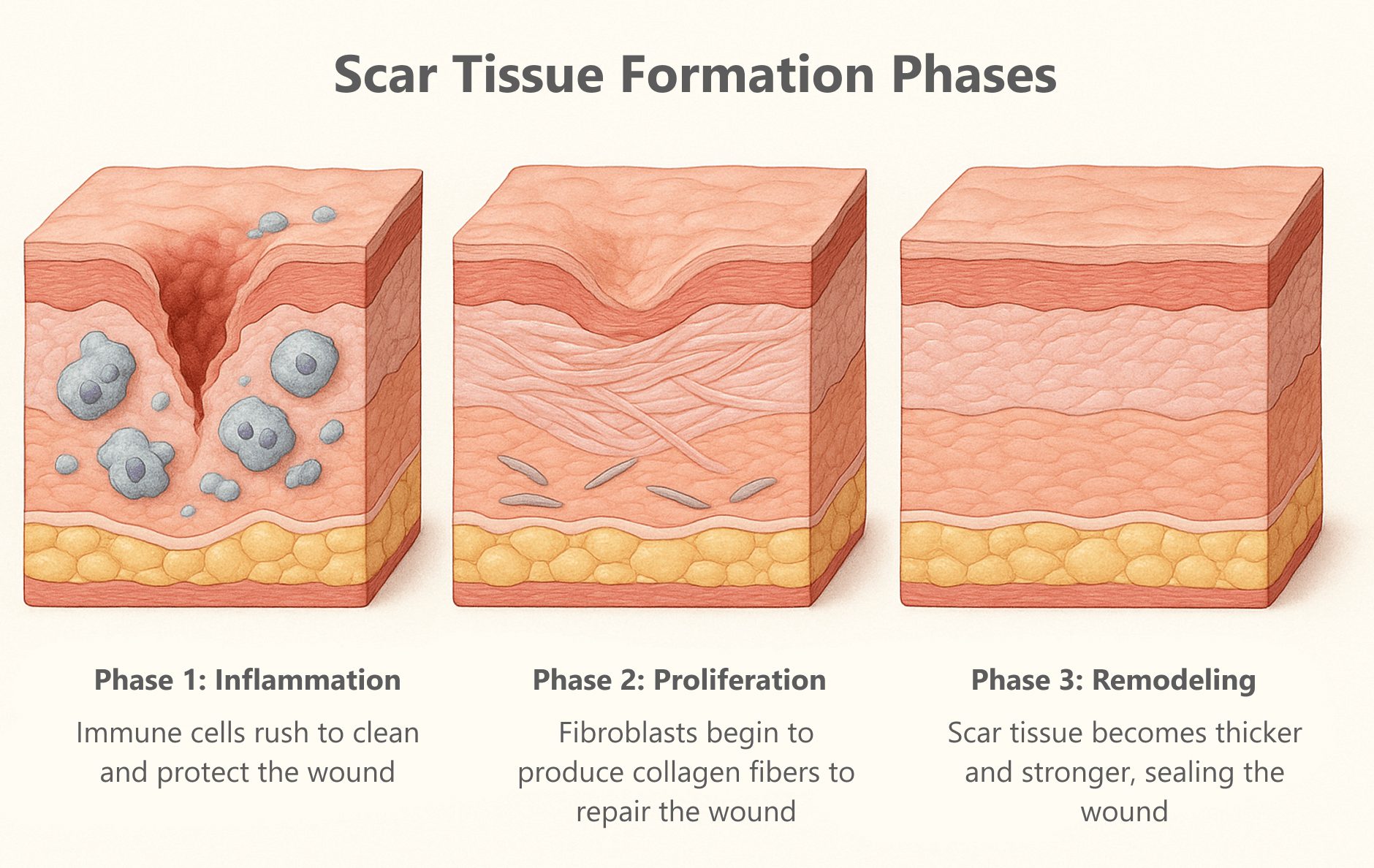
Sometimes during the healing process there is excessive collagen production, creating raised and thickened hypertrophic scars that may itch and feel tight. Keloids are abnormal scars that extend beyond the wound’s edges, forming raised, hard, irregularly shaped tissue. Keloids can continue to grow over time, even after the wound is sealed. Both hypertrophic scars and keloids can cause pain, restricted mobility, and cosmetic issues. When formed internally, they can adhere to other structures, creating adhesions that impair normal mobility and function.
While there is very good evidence that supports shockwave therapy as a treatment for keloids and hypertrophic scars, focal shockwaves are contraindicated for treatment of abdominal scars and adhesions due to the risk of damaging visceral organs. At the same time, radial shockwaves, while safe, do not penetrate deep enough to affect abdominal scar tissue.
Scar tissue does not arise out of nowhere – it only forms when soft tissues are wounded by surgery or trauma. In the abdomen, post-surgical scar tissue is challenging to treat for fear of damaging vulnerable abdominal organs. The abdominal cavity not only houses the visceral organs, but features a complex convergence of bones, muscles, nerves, and blood vessels that serve to produce movement and mediate force transfer between the upper and lower body – a critical role in any type of physical activity.
Fascia is a tough web of connective tissue, present throughout the body, that encases and connects muscles, bones and organs. Healthy fascia is slippery and elastic, enabling the body’s structures to glide without friction while working with muscles to guide and control movement. Together, muscles and fascia form the myofascial system, creating a balanced state of elastic tension called biotensegrity. When injuries occur – whether from trauma or surgery – biotensegrity is disrupted, altering muscle coordination patterns and impairing functional mobility.
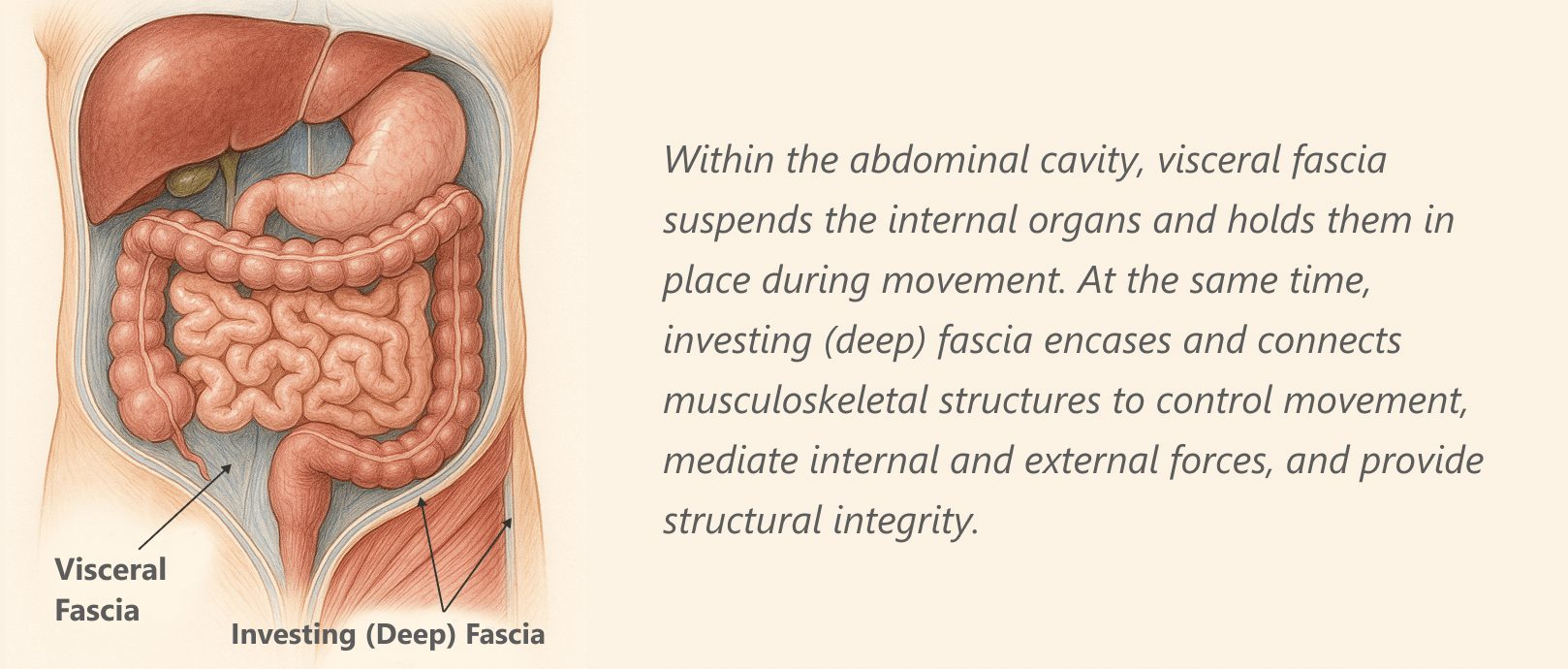
Within the abdominal cavity, visceral fascia suspends the internal organs and holds them in place during movement. At the same time, investing (deep) fascia encases and connects musculoskeletal structures to control movement, mediate internal and external forces, and provide structural integrity.
When fascia is damaged, it can become densified and sticky, and over time it can form abdominal adhesions that interfere with biotensegrity and impair abdominal motility. Once densified fascia turns into scar tissue it cannot be reversed, but there exist holistic therapies that can reduce the size of scar tissue, improve its pliability, and help to modulate pain.
Surgery-related adhesions are more likely to develop complications compared to other causes, and some can be life-threatening. Adhesion-related symptoms and complications can arise months or even decades after surgery.
Surgeries with a high risk of adhesion formation include:
Abdominal adhesions can cause chronic abdominal pain, bowel obstruction, female infertility and male reproductive disorders. Such issues are often addressed with additional surgeries, worsening the patient’s condition and increasing the risk of morbidity and mortality.
Complications of intra-abdominal adhesions include:
According to one source, abdominal adhesions cause 65% to 75% of small bowel occlusions, and 15-20% of female infertility. In some cases, abdominal adhesions can cause back pain and pelvic disorders due to their restrictive effect on biomechanics in the lumbopelvic region. They may also cause gait deficits and postural issues.
Adhesions can cause life-threatening intestinal obstructions that require immediate medical intervention. Adhesions and scar tissue can create a difficult environment for future surgeries, prolonging the length and complexity of procedures, and extending recovery time for the patient.
Some medical practitioners are quick to conclude that post-surgery abdominal complaints are caused by abdominal adhesions, but jumping to conclusions can lead to misdiagnosis and ineffective treatment that can worsen the patient’s condition. For confirmation, imaging modalities like CT scan, MRI and diagnostic ultrasonography are used to identify adhesions and their related complications.
To determine the most effective imaging technique for intra-abdominal adhesions, one team of researchers surveyed electronic databases to compare the efficacy of MRI, CT, and ultrasonography, in terms of overall accuracy. The review covered 25 studies and a total of 2195 patients. Of the three modalities, MRI and ultrasound were shown to have the best track records, with overall accuracy ranging from 79-90% for MRI, and 76 -100% for ultrasound, while CT scan showed an accuracy of only 66%..

For adhesion detection, ultrasound has distinct advantages over MRI:
Some medical doctors attempt to release adhesions via laparoscopic or open abdominal surgery, but surgery to treat adhesions can actually cause new adhesions to form. Holistic physical therapy for abdominal adhesions uses non-invasive alternative approaches to break up scar tissue and release adhesions while enhancing the integrity of associated tissues.
Alternative approaches for safe and effective adhesion therapy include:
The Stecco method of fascia manipulation involves deep friction that heats up tissues and stimulates mechanical action. When performed by a trained professional, Stecco fascia manipulation is a fantastic and evidence-based methodology for breaking up scar tissue and releasing adhesions. Regenerative technologies are often used in conjunction with Stecco to release abdominal adhesions. Patients often report immediate pain relief after a single Stecco session.
INDIBA therapy is an extracorporeal (outside the body) adhesion treatment approach that helps to restore the ionic charge of damaged cells. When used in conjunction with Stecco myofascial release and radial shockwave therapy, INDIBA helps to accelerate tissue healing at the cellular level.


Radial ESWT is an evidence-based technology that can be highly effective for treating keloids and hypertrophic scars, but radial waves do not penetrate deep enough to reach intra-abdominal adhesions. Nevertheless, radial shockwaves can help to loosen invested and visceral fascia, thereby enhancing mobility. Radial shockwaves also stimulate the growth of new microscopic blood vessels in the affected tissue.
Injecting substances such as corticosteroids, dextrose, or hyaluronic acid can help to normalize fascial tissue and break up intra-abdominal adhesions, especially when combined with other methodologies. However, blind injections carry risks of penetrating nerves and blood vessels while missing the targeted tissues altogether. For best results, needling procedures should be performed under the guidance of high-resolution ultrasound.


Abdominal adhesions from previous surgeries can make new procedures more complicated to perform, significantly increasing the patient’s risk of injury and infection, and prolonging the recovery period. Adhesions can complicate or even prohibit procedures like diagnostic ultrasonography, in-vitro fertilization, chemotherapy and kidney dialysis.
Recent research has shifted focus from treatment to prevention, to find effective ways to avoid future complications related to existing adhesions. Measures like optimizing patient health and nutrition status prior to surgery, and using ultrasonography to guide surgical procedures, are steps in the right direction. Precise and meticulous surgical technique is key to preventing adhesion formation.
Successful abdominal adhesion treatment begins with a thorough and accurate diagnosis. The clinic at NYDNRehab features the most advanced high-resolution diagnostic ultrasonography available. Dr. Kalika is a recognized expert in diagnostic ultrasound, with multiple scientific publications to his credit. Our clinic features the latest regenerative technologies, orthobiologic procedures, and evidence-based therapies
for treating scar tissue and adhesions. Our expertise in myofascial release techniques and visceral manipulation therapy is second to none.
If you have had abdominal surgery – either recently or in the past – and are suffering from abdominal pain, obstruction, or restriction, you may have developed abdominal adhesions that won’t go away on their own. Contact NYDNRehab today for accurate diagnosis and state-of-the-art abdominal adhesion therapy in NYC.
Dr. Lev Kalika is a world-recognized expert in musculoskeletal medicine. with 20+ years of clinical experience in diagnostic musculoskeletal ultrasonography, rehabilitative sports medicine and conservative orthopedics. In addition to operating his clinical practice in Manhattan, he regularly publishes peer-reviewed research on ultrasound-guided therapies and procedures. He serves as a peer reviewer for Springer Nature.
Dr. Kalika is an esteemed member of multiple professional organizations, including: