Tendon Pain and the Human Brain
When any area of your body is injured, you naturally and subconsciously shift weight-bearing loads to other body structures to alleviate pain and allow for healing. In people with peripheral tendinopathy, persistent chronic pain from injury or overuse elicits complex corticospinal and neuromuscular adaptations in response to altered loading patterns.
While those adaptations may be beneficial in the short term, they often remain long after injured tissues have healed, creating inefficient motor patterns that reduce performance and increase injury risk. In the past, most research and treatment programs for tendinopathy have focused on muscle and tendon strength, while largely overlooking motor control issues that stem from the brain.
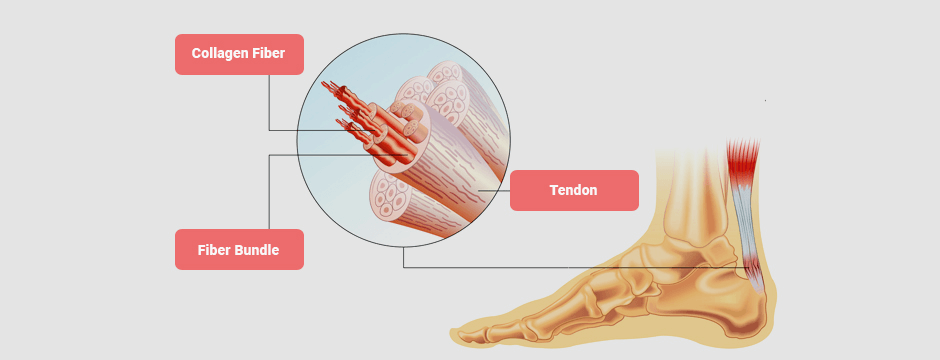
Loading Capacity of Tendons
Tendinopathy is a broad term that refers to tendon pain and/or dysfunction, with or without structural damage. Athletes with tendinopathy experience load-dependent localized tendon pain, coupled with reduced tendon function.
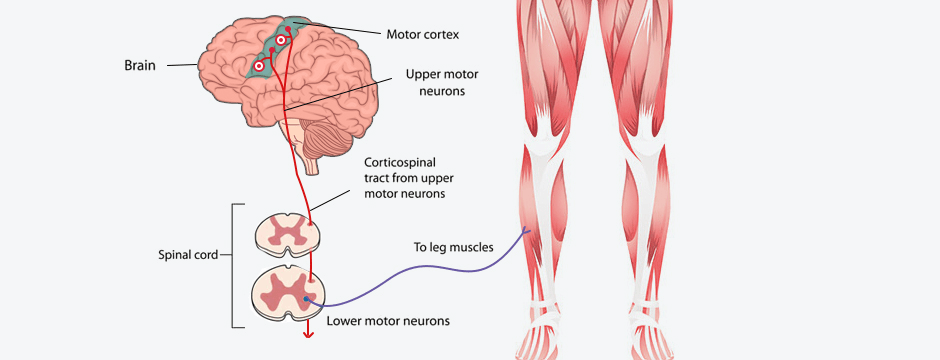
Tendons are highly adaptable to load-bearing activities, but they have a limited load capacity. Load-induced adaptations take place in both the structures of the tendon itself, and in the corticospinal tract, a segment of the central nervous system that begins in the cerebral motor cortex and ends at the lower motor neurons of the spinal cord.
When the load capacity of a tendon is exceeded, it can become injured and dysfunctional. This can in turn incite changes in the corticospinal tract. In the past, research on tendinopathy and tendon dysfunction has largely centered on the tendons themselves, while ignoring changes at the spinal cord and brain level. But new research is unearthing the important connection between brain neuroplasticity and muscle and tendon function.
The Tendon-Brain Connection
Every possible movement of the limbs and trunk is regulated by the motor cortex of the brain. Movement is generated and controlled by both excitatory and inhibitory stimuli. Explained simplistically, excitatory stimuli cause muscles to fire and contract, while inhibitory stimuli limit or inhibit the rate of contraction. In athletes with chronic Achilles or patellar tendinopathy, changes in the cerebral motor cortex interfere with their ability to regulate excitability and inhibition, causing loss of motor control.
Having excessive and simultaneous inhibition and excitation is like driving your car with one foot and the gas and one on the brake. With both stimuli in hyperactive mode, you may not be able to tell how much load is enough, or how much speed you need to reach a certain target, or know when to stop suddenly and begin again. Simultaneous excitation and inhibition of a motor unit can change the motor control patterns of the entire kinetic chain.
It is also possible that neuroplastic changes cause your sensory processors for proprioception, interception, vision, vestibular balance and hearing to not work properly, making it difficult for your brain to modulate sensory information.
New Strategies for Tendinopathy Treatment
The idea of treating tendinopathy by addressing neuroplastic changes is a relatively new concept, fostering a new rehabilitation approach known as tendon neuroplastic training. This approach incorporates motor control as a key strategy, in contrast to traditional treatment that focuses on muscle loading alone to treat tendon pain and dysfunction.
At NYDNRehab, we have advanced technologies and methodologies to test and treat tendinopathy that are rarely found in private rehab clinics. Our technologies are based on principles of neuroscience, and their effects go beyond those of traditional physical therapy.
Our tendon neuromodulation toolbox includes:
- Kineo Intelligent Load for optimal tendon concentric and eccentric loading, equipped with AI testing and feedback capabilities
- Proteus Motion system, for movement analysis and intelligent resistance-based workouts
- C.A.R.E.N, our computer assisted rehabilitation environment with a virtual reality feedback mechanism
State-of-the-Art Rehabilitation in NYC
The sports medicine team at NYDNRehab is always learning and acquiring new equipment and technologies, to offer our patients the most advanced evidence-based rehabilitation available. We use high-tech instruments to quantify individual human movement, taking the guesswork out of physical therapy and replacing it with actionable metrics.
In addition to injury rehab, we offer chiropractic care, sports performance assessment and training, 3D gait analysis and retraining, and much more. Our Telehealth services make it possible for our patients to stay on track with their therapy, even when they cannot make an in-person visit.
Resources Rio, Ebonie, et al. “Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review.” British journal of sports medicine 50.4 (2016): 209-215.
Te, Maxine, et al. “Primary motor cortex organization is altered in persistent patellofemoral pain.” Pain Medicine 18.11 (2017): 2224-2234.