ACL Surgery: Is it really necessary?
Ruptures of the anterior cruciate ligament, or ACL, are among the most common athletic injuries, estimated to total as many as 200,000 per year in the United States. Agility sports have the highest rates of injury, and female athletes have a higher rate of ACL ruptures than males. ACL injuries are especially common in field sports like football, soccer and rugby, and in court sports like basketball and volleyball. ACL rupture is also a common injury in downhill (Alpine) skiing.
The High Prevalence of ACL Tears
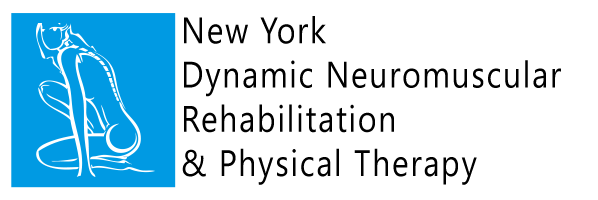
The cruciate ligaments of the knee connect the top of the tibia, or shin bone, to the underside of the femur, or thigh bone. They are supported and stabilized by the muscles and tendons that converge at the knee. The role of the anterior cruciate ligaments is to keep the tibia from sliding in front of the femur, which is why they are sometimes described as the seatbelts of the knee.
Everyday locomotor activities like walking, running or climbing stairs pose little danger to the ACLs. But during sports, when the athlete is leaping, landing, cutting and rotating on a planted foot, dynamic forces are at work to push the tibia out of position. If the forces are great enough, the ACL cannot withstand them, and rupture occurs. With modern athletes becoming bigger and faster, their knees are being subjected to increasingly greater forces.
Many ACL tears occur when the athlete’s hips are unnaturally rotated, amplifying the force loads on the knee. There is minimal muscle support for rotational movement at the knee, making the ACL more vulnerable to injury. The hamstring and quadriceps muscles are much more adept at protecting and supporting the collateral ligaments on the outside of the knee.
What Happens When You Tear Your ACL?
The moment an elite athlete ruptures and ACL, the clock begins ticking. The sooner the injury is treated, the sooner the athlete can return to play. The stakes are high in terms of money, team standing and the athlete’s future career. In such cases, reconstructive surgery within a few weeks is almost always the first line of treatment, followed by intensive physical therapy.
When stakes are lower, as with a recreational athlete, immediate reconstructive surgery is often foregone in favor of physical therapy, with the option of surgery later if conservative treatment is insufficient. Interestingly enough, research on the relative advantages of surgical vs nonsurgical treatment of ACL tears reveals there are few differences in long-term outcomes.
How Reconstructive Knee Surgery is Done
Anterior cruciate ligament reconstruction (ACLR) involves replacing the ruptured ligament with a section of tendon, usually taken from the patient’s own leg or from a cadaver. The patient’s own tissue is often taken from either the hamstring tendons, or from the patellar tendon below the knee. Most ACLRs are done arthroscopically, through small incisions. In the past, surgeons tried to repair the ACL by sewing it back together, but that approach was generally ineffective.
Some athletes who undergo ACLR followed by intensive physical therapy are able to return to sport within four to nine months, and most can return to play within a year. However, many factors help determine an athlete’s readiness to return to play:
- Degree of injury (full or partial tear)
- Relative stability of the knee pre-injury
- Length and scope of rehabilitative therapy
- Mental and emotional factors of the individual athlete
At the end of the day, rehabilitative therapy plays the greatest role in preparing the athlete to return to the playing field after ACLR. Athletes who are non-compliant with rehab protocols and fail to stay the course of the rehab program are more likely to be re-injured over the course of the following year.
Compelling Research Challenges the Need for ACL Reconstruction
The decision to perform reconstructive knee surgery after an athlete is injured is often emotionally charged. The media, sports fans and commentators, and coaches and team managers all contribute to the frenzy, making ACLR an imperative rather than an option. Yet research comparing the outcomes of surgery and rehabilitative physical therapy casts doubt on the tendency to perform surgery as a first line of treatment.
- A study by Swedish and Danish researchers followed 121 active adults with ACL tears. Half were randomly assigned to undergo both physical therapy and surgery. The other half had physical therapy only, with the option to have surgery later. Two years after their injuries, both groups saw substantial improvement in knee function. More importantly there were no major differences between the groups in terms of pain, inflammation and function, in both sports and activities of daily living.
- Another study of 143 patients with ACL injuries found little difference at the end of their course of treatment between those who had ACLR followed by physical therapy and those who had physical therapy alone.
Conservative Treatment Measures
While ligaments can be made stronger through physical activity, the ACL is difficult to isolate during exercise. Most physical therapy treatments are geared to strengthening the muscles and tendons that support the knee. For the greatest chances of returning to play with the least risk of re-injury, athletes should work with a therapy clinic that offers evidence-based rehabilitation.
Evidence-based ACLR rehabilitation includes pre-hab, followed by 3 post-surgery criterion-based phases, ending with a gradual return to sport only after satisfying functional performance criteria. With this approach, the athlete plays an active role in their own rehabilitation, providing feedback and input throughout the process. The protocol includes patient education, goal-setting and repeated functional testing and feedback.
Evidence-based rehab criteria include:
- Pain
- Effusion
- Range of motion
- Neuromuscular control, endurance, strength and power
- Movement patterns (walking, running, jumping and aport-specific movements)
- Sports performance (acceleration, agility, coordination, balance, endurance and sport-specific skills)
- Psychological readiness
The evidence-based approach treats athletes on a case-by-case basis, customizing the rehab process to the individual to ensure they are fully ready to safely return to play.
ACL Rehab in NYC
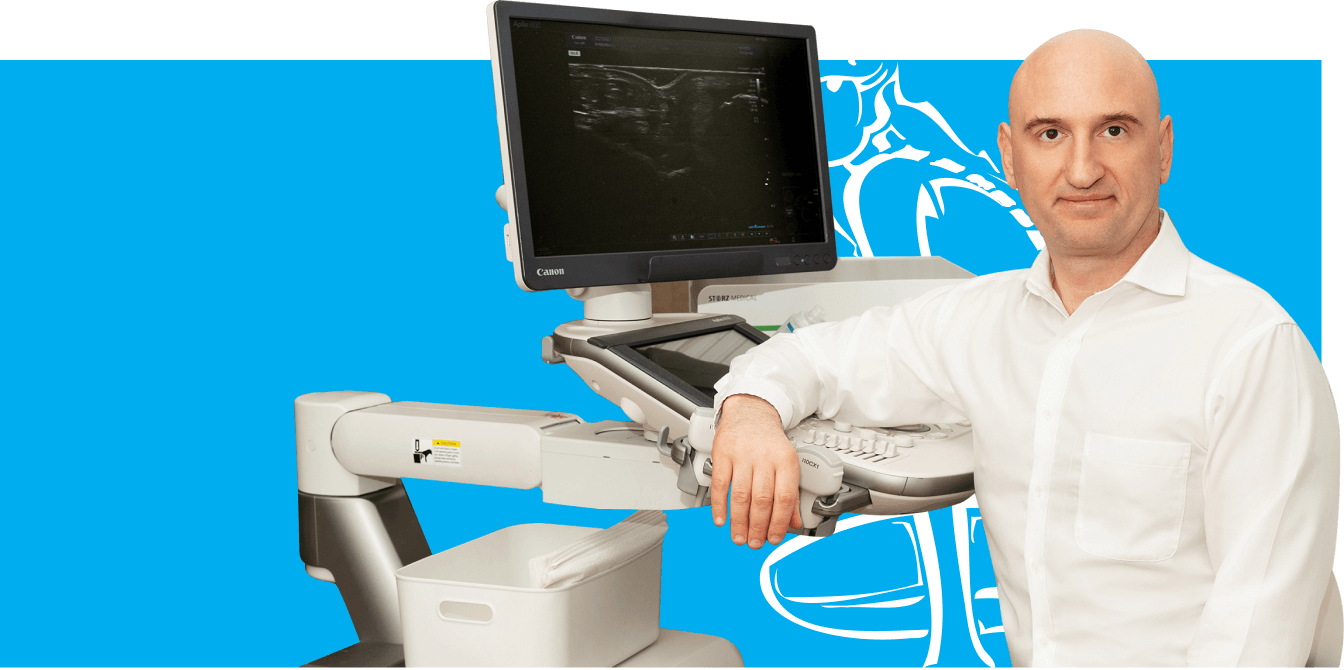
NYDNRehab provides chiropractic care and physical therapy in NYC, combining proven medical approaches with state-of-the-art solutions. Our sports performance specialists have the unique advantage of access to advanced technologies, customized software programs, and the capacity to formulate data-driven rehab protocols.
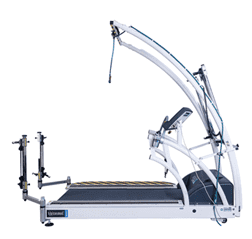
Our clinic houses technologies rarely found in private rehabilitation clinics, including:
- Alter-G anti-gravity treadmill
- Dual force plate technology
- 3D motion capture video
- C.A.R.E.N (computer-assisted rehabilitation environment)
- High resolution ultrasonography
By applying quantitative data derived from technological analysis, we are able to monitor your progress, modify your rehab protocol, and make accurate projections about your readiness to return to play. If you have an ACL injury and want to get back out there safely, with low risk of re-injury, come to NYDNRehab and get the best rehabilitative care in NYC.
Resources:
Grindem, Hege, et al. “Nonsurgical or surgical treatment of ACL injuries: knee function, sports participation, and knee reinjury: the Delaware-Oslo ACL Cohort Study.” The Journal of bone and joint surgery. American volume 96.15 (2014): 1233.
Grindem, Hege, Amelia JH Arundale, and Clare L. Ardern. “Alarming underutilisation of rehabilitation in athletes with anterior cruciate ligament reconstruction: four ways to change the game.” (2018): 1162-1163.
Myklebust, G., and R. Bahr. “Return to play guidelines after anterior cruciate ligament surgery.” British journal of sports medicine 39.3 (2005): 127-131.