What Gait Says About Aging and Brain Health
By the time we get to midlife, most of us have had an “Ah-hah” moment where we have considered our own mortality. While none of us can predict how or when we will meet our end, there are many things you can do now to influence how well your body ages over time. In fact, recent research suggests that how you walk at age 45 could help predict your cognitive health in the years to come.
Gait Analysis Applications
Your gait is defined by the way you walk and run. You can probably recognize familiar people from a distance, based on their gait, long before you see their faces. Gait analysis is a science that looks at all facets of human gait, including joint angles, muscle activation patterns, ground reaction forces and other measurable data. To give you an idea of how unique your gait is, gait analysis technology is now being used in China to identify individual citizens, much like facial recognition technology.
Gait analysis has many applications. It can help athletes fine-tune their performance, can be used to rehabilitate injuries and reduce their risk, and it can be used to assess and improve balance and stability in older adults. By extracting quantifiable data from technological tools, gait specialists can design rehabilitation programs that are specific to each individual patient.
The Link between Gait and Cognition
Impaired gait has always been associated with aging. Changes in gait over time are caused by multiple factors, including lifestyle behaviors, physical activity levels, changes in metabolic health, vision and hearing loss, pharmaceutical side effects, past injuries and a host of other variables. Deficits in gait increase the risk of falls and injury in older adults, and can lead to hospitalization, institutionalization and even death.
Gait performance falls under the umbrella of executive function, which governs planning, goal-based action and coordination of the complex factors involved in locomotion.
Multiple biological factors play a role in gait, including:
- Musculoskeletal fitness
- Cardiovascular fitness
- Vision
- CNS (central nervous system)
- PNS (peripheral nervous system)
- Cellular energy production
- Vestibular system
In older adults with impaired cognition, or dementia, changes in gait are even more profound. The term “senile gait” refers to the reduced stride and shuffling gait often observed in cognitively impaired patients. Correlations between cognitive impairment and deficits in gait are well established in scientific literature.
How Midlife Gait Predicts Cognition in Older Age
The concept of using current health markers to predict potential future health issues is nothing new. Health care providers have been doing it for decades to predict lung cancer, heart disease, diabetes and other metabolic disorders, based on a patient’s lifestyle behaviors, blood serum profile and vital statistics.
As gait analysis technology evolves, scientists have begun to recognize that certain gait characteristics earlier in life may foreshadow cognitive decline over time. In fact, evidence suggests that gait deficits have their origins in the early developmental stages of childhood, when changes in the brain and central nervous system coincide with an infant’s mastery of crawling, standing, walking and running.
Gait Analysis and Neurodegenerative Disorders
Gait analysis at midlife is not only being used to predict potential cognitive decline, but specific gait patterns can now help differentiate between different types of dementia. By analyzing gait speed, step length variability and asymmetries in step time, up to 60 percent of dementia subtypes can be accurately identified.
For example, patients with Alzheimer’s disease have gait patterns distinct from those with Lewy body dementia. Because the two conditions are difficult to tell apart in the early stages, gait analysis can play an important role in helping patients, families and health care providers make important decisions about treatment and long-term care.
Data-Based Gait Analysis in NYC
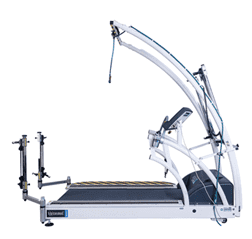
There are many tests and assessments used to analyze gait, but many of them only give a generalized idea of gait deficits. An accurate and detailed data-based gait analysis requires advanced technological tools coupled with sophisticated computer software. NYDNRehab is one of the only private clinics in the United States equipped and trained to conduct research-grade gait analysis.
Our technological toolkit includes:
- 3D motion capture video
- Force plate technology
- Vestibular balance technology
- C.A.R.E.N. (computer assisted rehabilitation environment)
- Virtual reality feedback
Whether you are concerned about aging, want to improve your balance, or simply want to improve your gait to perform better and prevent injury, the team at NYDNRehab has the expertise and technology to provide you with accurate results and innovative interventions. Contact us today, and take the first steps toward healthy aging and a better long-term quality of life.
Resources
Conceição, Miguel S., and Carlos Ugrinowitsch. “Exercise with blood flow restriction: an effective alternative for the non‐pharmaceutical treatment for muscle wasting.” Journal of cachexia, sarcopenia and muscle 10.2 (2019): 257-262.
Kim, SoJung, et al. “Effects of short term low intensity resistance training with blood flow restriction on bone markers and muscle cross-sectional area in young men.” International Journal of Exercise Science 5.2 (2012): 6.
Manini, Todd M., and Brian C. Clark. “Blood flow restricted exercise and skeletal muscle health.” Exercise and sport sciences reviews 37.2 (2009): 78-85.
Ohta, Haruyasu, et al. “Low-load resistance muscular training with moderate restriction of blood flow after anterior cruciate ligament reconstruction.” Acta Orthopaedica Scandinavica 74.1 (2003): 62-68.
Pearson, Stephen John, and Syed Robiul Hussain. “A review on the mechanisms of blood-flow restriction resistance training-induced muscle hypertrophy.” Sports medicine 45.2 (2015): 187-200.
Vechin, Felipe C., et al. “Comparisons between low-intensity resistance training with blood flow restriction and high-intensity resistance training on quadriceps muscle mass and strength in elderly.” The Journal of Strength & Conditioning Research 29.4 (2015): 1071-1076.