Are You at Risk for Patellofemoral Pain?
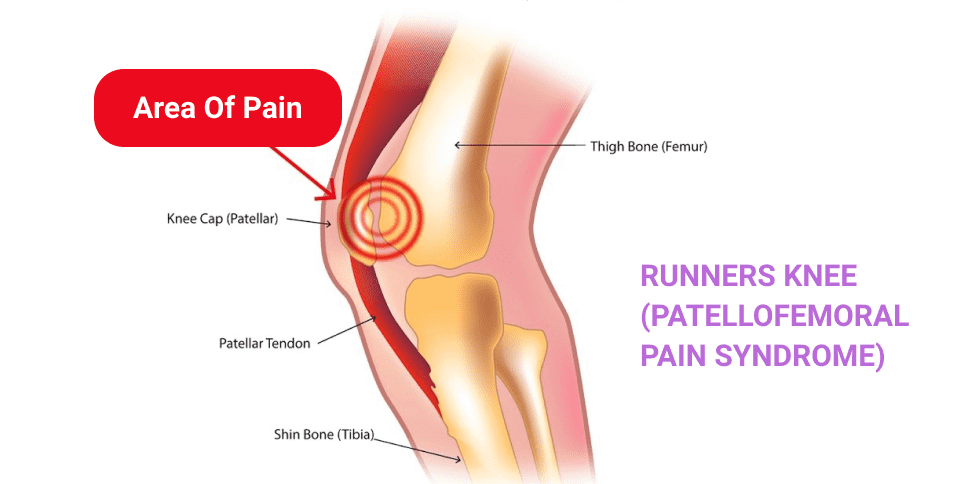
Patellofemoral pain syndrome (PFPS) is a relatively common athletic injury, seen mostly among younger athletes in their teens and 20s, with females being at greater risk. Non-athletic populations also experience PFPS, but to a much lesser degree. PFPS affects the knee, where the femur (thigh bone) and patella (kneecap) converge.
PFPS is sometimes called “jumper’s knee” or “runner’s knee” because it occurs most often in sports that involve jumping, running, pivoting and cutting, like basketball, volleyball, track or cross-country. PFPS is the most common overuse injury in runners, and often becomes a chronic complaint among those afflicted. Yet not all athletes experience PFPS, and some are more prone to the condition than others.
Symptoms of PFPS
The knee is a complex structure, capable of withstanding massive force loads during physical activity. Jumping, landing and repetitive impact during running challenge the knee’s capacity to withstand stress, and PFPS is often the result.
Common symptoms of PFPS include:
- Dull achy pain under or surrounding the kneecap, with no specific onset.
- Pain with activities that load the knee while bent, like climbing stairs or squatting.
- Pain after prolonged sitting in a bent-knee position.
- Popping and crackling sounds or sensations when climbing stairs or standing from a seated position.
- Pain while running and jumping.
- Increased pain at higher intensities, or on unforgiving surfaces.
Since other more serious conditions can mimic the symptoms of PFPS, it is important to get an accurate diagnosis from a sports medicine professional.
Factors that Contribute to PFPS
The specific underlying causes of PFPS are difficult to identify, and a number of factors may be at play. Because the onset of PFPS cannot be associated with a specific incident, unlike an ACL tear or an Achilles rupture, the specific mechanisms of pain are hard to pinpoint.
While anyone can suffer from PFPS, there are certain factors that may predispose an individual to the condition:
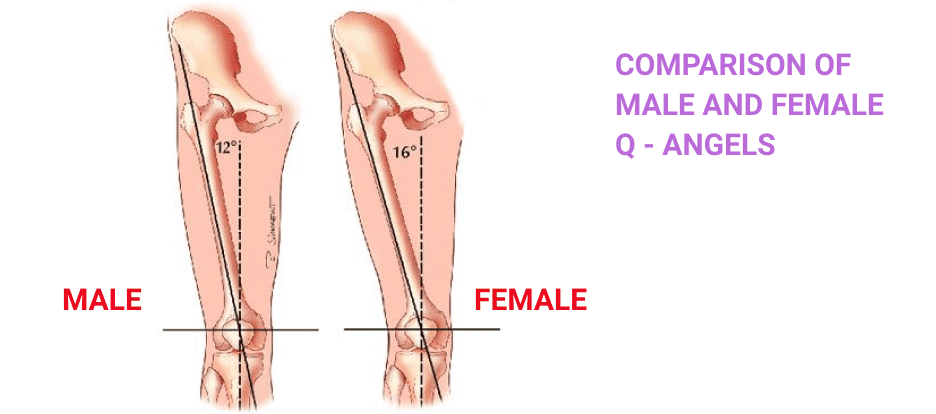
- Quadriceps angle (Q-angle) alignment: PFPS accounts for 33% of all knee injuries in female athletes, compared to 18% in males. One factor contributing to this disparity may be a wider pelvis in females, which affects the alignment of the hip and knee joints, creating a larger Q-angle. However, there are conflicting views in the sports medicine community about the relationship between Q-angle and PFPS.
- Deficient kinematics and compensatory motor patterns: Faulty motor patterns and inefficient joint angles in the hip, trunk, core and foot can cause damaging force loads on the knee and increase the risk of PFPS. Also, pain in any region can cause compensation patterns, where movement is altered to reduce load on the painful area, shifting force loads at the knee and leading to injuries like PFPS.
- Deficient neuromuscular control of the lower extremities: Efficient pain-free movement calls for reflexive timing of muscle contractions and the ability to stabilize muscle groups during weight-bearing activities. Weakened muscles often underperform, causing load forces to shift and increasing stress at the knee. This is a training issue that can be identified and corrected.
It is important to note that young athletes are less likely to get adequate coaching on biomechanics, for a number of reasons. Many will fail to excel at a sport, and most are unlikely to progress to collegiate or professional sports. Few youth programs have the resources, human or monetary, to provide individualized coaching for every player. Yet poor motor mechanics early on can lead to the formation of bad habits, which in turn lead to injuries.
Diagnosis of PFPS
PFPS is a medical condition that should be diagnosed by a sports medicine physician. They will ask questions about your pain onset and symptoms, and perform a physical exam. You will be asked about your training program, any changes made in training or activity type or intensity, and other relevant questions. Strength and jump tests may be included in the diagnostic process to identify areas of weakness and mechanical errors.
Since other more serious injuries mimic PFPS symptoms, diagnostic ultrasound imaging may be performed to rule out conditions such as patellar dislocation, instability or damaged cartilage.
Treatment Options for PFPS
In addition to pain management strategies like rest, icing and NSAIDS like ibuprofen or naproxen, physical therapy is the primary treatment for PFPS. After a thorough assessment to identify weakened muscles and biomechanical errors, your therapist will design an exercise program to strengthen and balance muscles around your hip, quadriceps and hamstrings. A sports physical therapist will also evaluate dynamic joint angles and loading patterns before, during and after treatment, to make corrections and measure progress.
Knee Pain Treatment in NYC
At NYDNRehab, we use the most advanced technologies to quantify measurements of joint angles, force distribution and motor efficiency. A quantifiable baseline provides us with the specific data we need to accurately identify the source of knee pain. We then create an individualized treatment plan and measure its effectiveness along the way, to correct mechanical errors and instill efficient motor patterns.
Our sports medicine team is dedicated to not only eliminating your knee pain, but to correcting the issues that caused it. Our end goal is to improve your performance and reduce your risk of future injuries. Don’t let knee pain take you out of the game. Contact NYDNRehab today, and reach your full performance potential, pain-free.
Resource
Halabchi, Farzin, et al. “Patellofemoral pain in athletes: clinical perspectives.” Open access journal of sports medicine 8 (2017): 189.