
Hip impingement, more formally known as femoroacetabular impingement (FAI), is a painful condition that can get worse if it is not treated properly. Normally, the head of the hip bone, or femur, is a rounded knob that fits into the acetabulum, a socket in the side of the pelvis. In hip impingement, bone spurs develop in the joint and cause the bones to scrape together instead of rotating smoothly.
If the spurs are on the head of the femur, it is called a cam impingement, while if they form around the acetabulum, it is called a pincer impingement. It is also possible for spurs to form on both, resulting in a combined impingement. Regardless of where the spurs form, they cause stiffness and pain in the hip and groin. Some doctors believe that if left untreated, the spurs can tear into the cartilage that supports and lubricates the bones, resulting in arthritis of the hip. Hip impingement is a relatively new diagnosis, discovered about ten years ago. But is this surgery really necessary, or are there less extreme ways to deal with this condition?
The actual cause of hip impingement is not known. It may be genetic, or the result of poor bone formation as a child. Strenuous exercise often puts stress on the hips and can lead to spurs forming earlier, but exercise alone does not cause impingement.
Some physicians recommend surgery for hip impingement to remove the bone spurs. However, there is increasing evidence that removing the spurs is simply treating the symptoms, not the underlying problem.
A 2013 paper by a team of physicians in Norway showed that pincer impingement did not lead to arthritis — in fact, the bone spurs formed to protect the joint from stresses that might have damaged the hip. If this is true, then removing the spurs is a bad idea and may lead to more severe hip injuries over time. This doesn’t mean you have to live with the pain of hip impingement, though.
Research has shown that it’s actually possible to lessen the severity of hip impingement through activity modification, physical therapy, and exercise. Another study of 50 patients with hip impingement proved that posture made a difference. Standing or sitting with the pelvis tilted forward makes the impingement more severe, while tilting the pelvis backward means less impingement and less pain.
This research into pelvic tilt suggests the true cause of hip impingement may be poor posture, a result of age, obesity, and/or back pain. These conditions can cause the forward tilt of the pelvis that stresses the hips and may lead to the formation of bone spurs. If this is true, then surgery may be unnecessary to treat impingement. In fact, surgery may even make the problem worse by removing the body’s attempt to provide extra support to the overstressed hips.
Simply changing your activities to avoid movements that stress your hips, allowing them to rest and heal, can be enough in mild cases. If this is not enough, impingement can be dealt with through exercises that strengthen your hips, upper legs, groin, and abdomen. This will enable improved posture, so the pelvis can return to its natural tilt and the pain of impingement can be relieved.
Even if you have limited mobility due to age or other conditions, a physical therapist or orthopedic specialist will be able to work with you to design a regimen of stretches and exercises to strengthen the muscles of your core and legs. Don’t assume that surgery is the only, or even best, solution for any kind of joint pain. Our modern lifestyle frequently subjects the musculoskeletal system to unnecessary and unnatural stresses and help to fix hip impingement without surgery. Identifying those stresses, and knowing how to ease them, is a key to keeping strong, healthy joints even later in life.

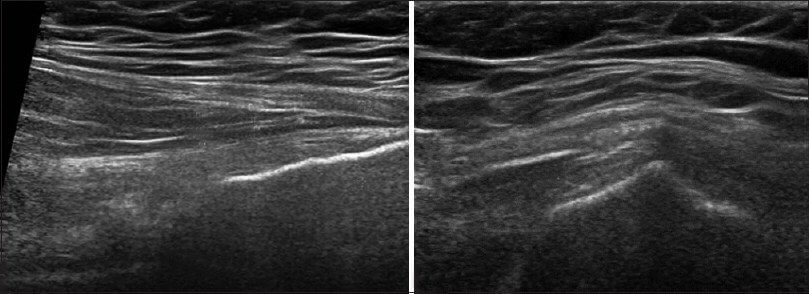
A clinical exam and diagnostic ultrasound imaging can help your therapist pinpoint the exact location and cause of your hip and groin pain.
Ultrasound enables you and your therapist to view the hip and groin region in real time, while in motion. In addition to ultrasound, video gait analysis can help us identify faulty movement mechanics that contribute to hip and groin pain. Once the exact cause is determined, an effective treatment plan can be initiated.
Please explore more advanced diagnostic option unavailable anywhere else:

Our testing protocol includes:
Combined lumbopelvic hip stability test using DLEST methodology with C.A.R.E.N., our computer assisted rehab environment
Hip joint stability test using DLEST methodology with C.A.R.E.N.
3D star excursion banner test (SEBT) for assessing the involvement of the hip joint and muscles in postural stability
3D gait or running analysis
3D kinematic joint angle analysis during a squat, lunge, drop jump and pelvis on hip rotation
Rehabilitative ultrasonography for viewing intrinsic hip stabilizing muscle activation patterns
Dr. Lev Kalika is a world-recognized expert in musculoskeletal medicine. with 20+ years of clinical experience in diagnostic musculoskeletal ultrasonography, rehabilitative sports medicine and conservative orthopedics. In addition to operating his clinical practice in Manhattan, he regularly publishes peer-reviewed research on ultrasound-guided therapies and procedures. He serves as a peer reviewer for Springer Nature.
Dr. Kalika is an esteemed member of multiple professional organizations, including: